Editorial notice
The formation of endocrinology as an independent medical discipline was preceded by the accumulation of medical experience during many centuries. The medicine of the ancient times was developing on the basis of continuity according to the basic principle «relata refero» (I tell what I have been told). Medicine and pharmacy in the countries of the ancient world had many similarities, but at the same time each civilization had its own geographical, cultural and historical particularities. The pathology of the thyroid was among the most studied pathologies in Ancient world. There are frequent mentions of the endemic goiter in the works of doctors from Ancient China, Ancient India and Ancient Greece.
Although the link between iodine and the thyroid was not known, algae and dried sea sponges were using for treating swollen neck.
There are many descriptions of neuroendocrine pathologies in historical sources, for example the Bible describes gigantism and the Talmud — hypoprolactinaemia.
Special attention was paid to the study of diabetes mellitus, although the pathogenesis and treatment of the disease remained unknown until the 20th century.
Clinical endocrinology
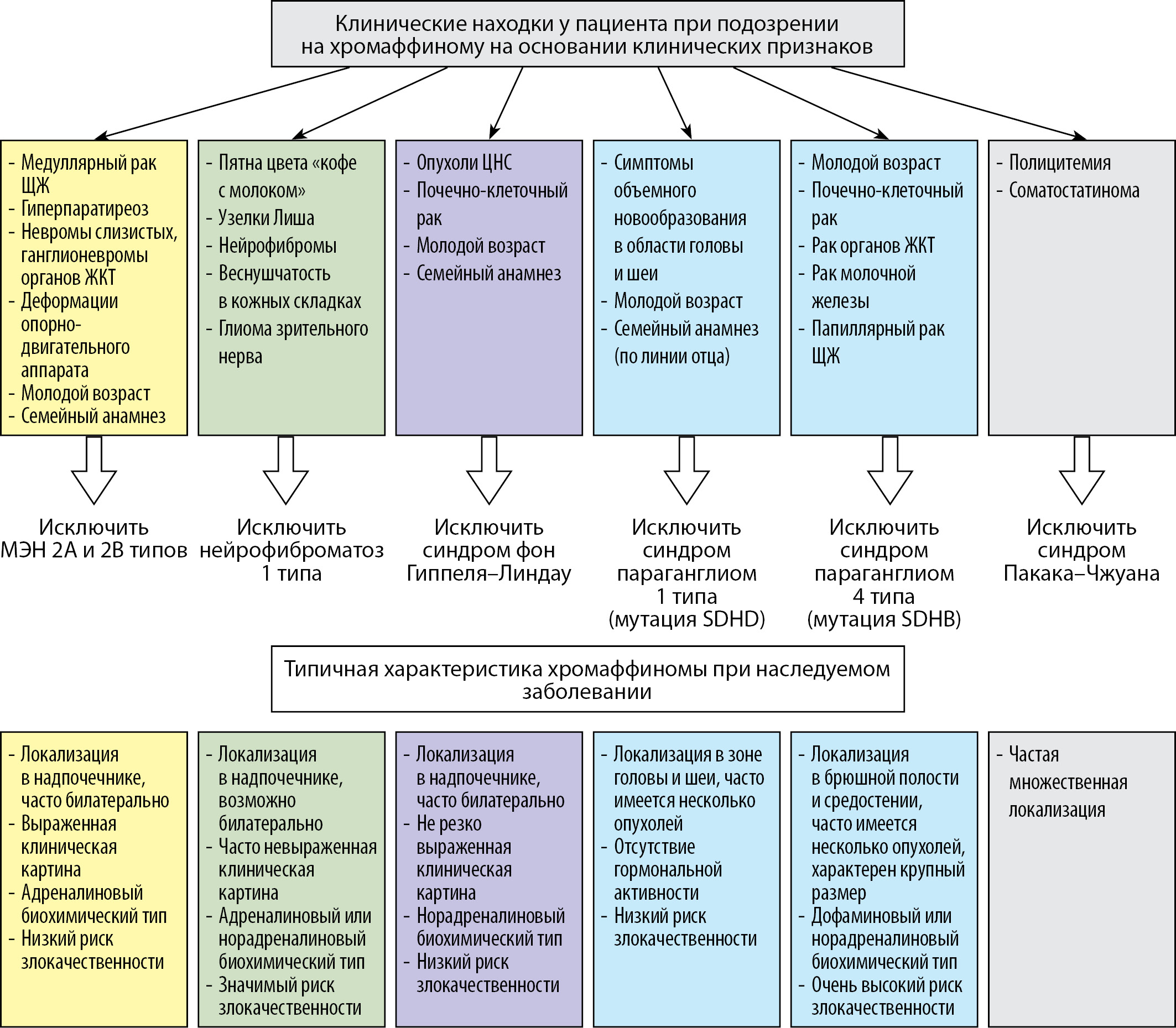
The widespread introduction of genetic testing in recent years has made it possible to determine that more than a third of cases of pheochromocytomas and paragangliomas (PPPGs) are caused by germline mutations. Despite the variety of catecholamine-producing tumors manifestations, there is a sufficient number of clinical and laboratory landmarks that suggest a hereditary genesis of the disease and even a specific syndrome. These include a family history, age of patient, presence of concomitant conditions, and symptoms of the disease. Considering that each of the mutations is associated with certain diseases that often determine tactics of treatment and examination of a patient, e.g. high risk of various malignancies. Awareness of the practitioner on the peculiarities of the course of family forms of PPPGs will allow improving the tactics of managing these patients.
The article provides up-to-date information on the prevalence of hereditary PPPGs. The modern views on the pathogenesis of the disease induced by different mutations are presented. The main hereditary syndromes associated with PPPGs are described, including multiple endocrine neoplasia syndrome type 2A and 2B, type 1 neurofibromatosis, von Hippel-Lindau syndrome, hereditary paraganglioma syndrome, as well as clinical and laboratory features of the tumor in these conditions. The main positions on the necessity of genetic screening in patients with PPPGs are given.
BACKGROUND. The standard treatment for hypothyroidism is levothyroxine (LT4), which in the Republic of Belarus is available in tablet form whereas liothyronine (LT3) is not registered, but patients can purchase them on their own abroad.
AIM. This study aimed to investigate Belarusian endocrinologists’ attitude of thyroid hormones in hypothyroid and euthyroid patients.
MATERIALS AND METHODS. An online survey was conducted, for which members of the Belarusian Medical Association of Endocrinology and Metabolism were invited by posting information in the group chat and by e-mail. The research period was from October 1 to December 26, 2020. 210 questionnaires were received, 146 of which were used.
RESULTS. The majority of participants, 145 (99.3%), indicated that they were using LT4 as the first-choice drug for the treatment hypothyroidism. Sixty-one (41.8%) doctors answered that LT3 + LT4 combination likely can be used in patients with long-term untreated hypothyroidism and 15 (10.3%) — in patients with persistent symptoms of hypothyroidism, despite biochemical euthyroidism on therapy LT4. Over half of the respondents 84 (57.5%) answered that thyroid hormone therapy was never indicated for euthyroid patients, but 50 (34.2%) would consider it for female infertility with high level of thyroid antibodies and 36 (24.7%) for simple goiter growing over time. In various conditions that could interfere with absorption of LT4, most responding Belarusian endocrinologists do not expect a significant difference with different formulations (tablets
+“I do not expect major changes in different forms” vs. “soft gel capsules”+“liquid solution”; p <0.001). Persistent symptoms of hypothyroidism on the background of LT4 replacement therapy with the achievement of the target TSH can mainly be caused by psychosocial factors, concomitant diseases, unrealistic patient expectations, chronic fatigue syndrome, and the burden of chronic disease.
CONCLUSION. The method of choice of Belarusian endocrinologists in the treatment of hypothyroidism is LT4 replacement therapy, but the appointment of LT4 + LT3 combination therapy can be considered in certain clinical situations. As a rule, endocrinologists do not prescribe LT4 in patients with euthyroidism and do not expect a significant difference when using other forms of levothyroxine.
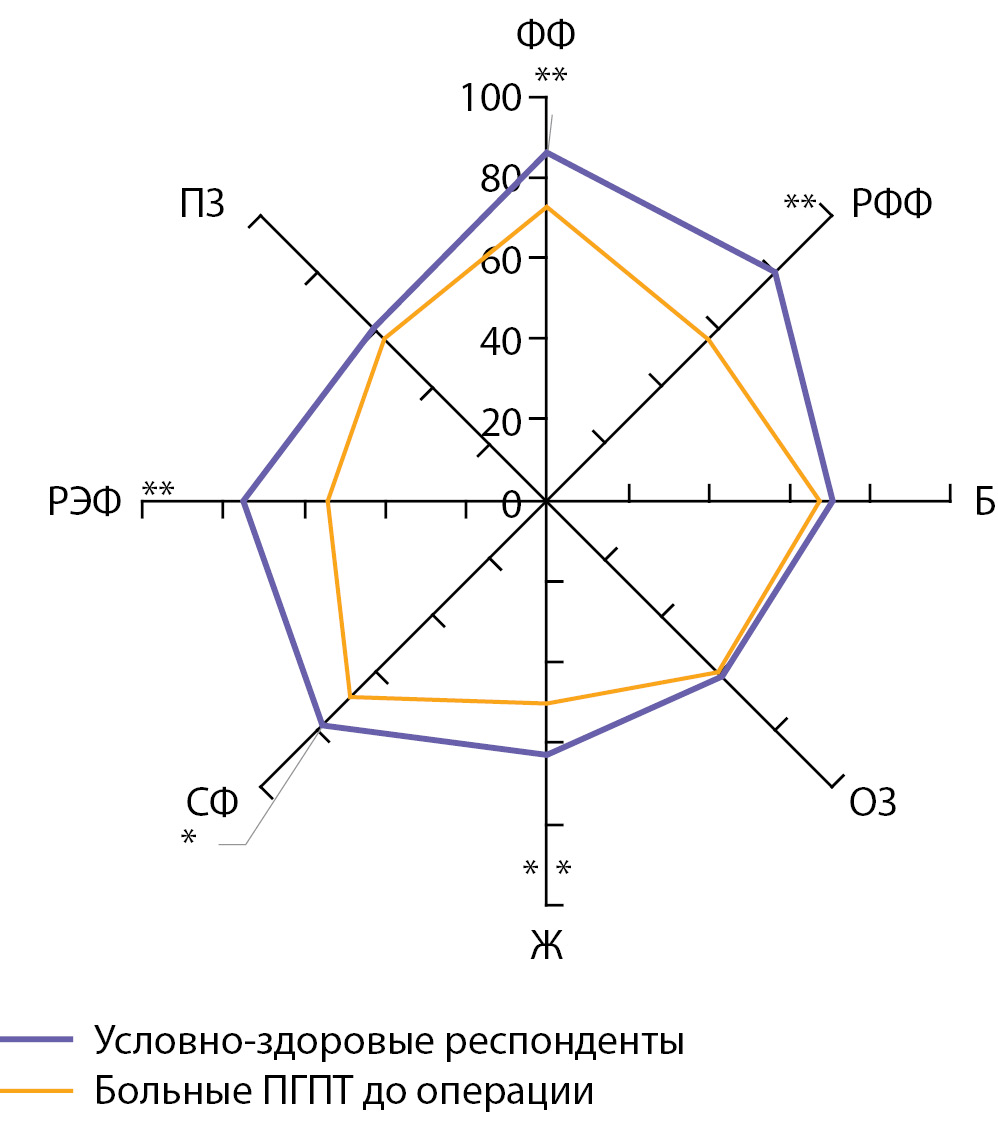
BACKGROUND: For a comprehensive assessment of the effect of surgery in patients with primary hyperparathyroidism (PHPT), as well as for monitoring the condition of patients after treatment, it sounds reasonable to evaluate quality of life (QoL) and symptoms in PHPT patients before and after surgery.
AIM: The aim of this study was to assess changes in the QoL and symptoms in patients with PHPT after surgery.
MATERIALS AND METHODS: During prospective observational study, patients filled out QoL questionnaires and evaluated the presence and severity of their symptoms prior to parathyroidectomy (PTE) and 3, 12 months after surgery. Statistical analysis included the following methods: Student’s t-test or Wilcoxon’s non-parametric test, the generalized estimating equations (GEE), correlation analysis, χ2 and McNemar tests.
RESULTS: The study included 72 patients (mean age 52 years, 97.2% female) with symptomatic (68.1%) and asymptomatic (31.9%) PHPT. Before surgery patients with PHPT exhibited significantly decreased role functioning, physical and social well-being, and vitality. Half of PHPT patients experienced moderate-to-severe symptoms such as weakness, fatigue, loss of concentration, mood changes, as well as joint and bone pain; the association between symptoms experienced and the extent of QoL impairment before surgery was shown. Three months after PTE improvement in both physical and psychological components of QoL was shown. Positive QoL changes were demonstrated in patients with both symptomatic and asymptomatic PHPT and they preserved for 12 months after surgery. Also within 12 months after PTE significant decrease in PHPT-associated symptoms such as weakness, fatigue, loss of concentration and mood changes was found.
CONCLUSION: The results obtained demonstrate efficacy of PTE from the patient’s perspective and confirm the value of QoL assessment in PHPT patients in management of this patients’ population both for decision making and for evaluation of benefits of surgery and the degree of recovery of patients at long term follow-up.
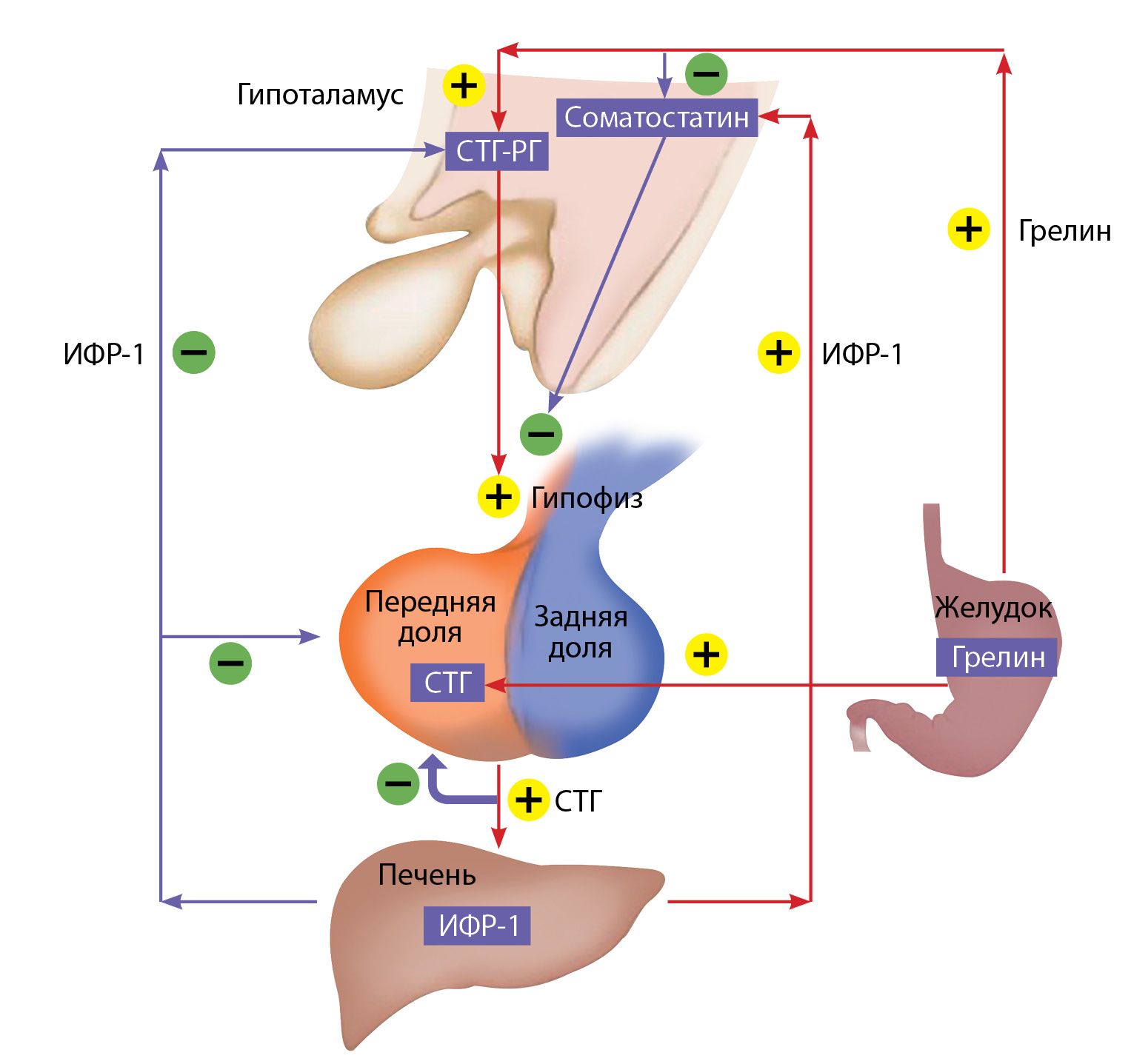
Acromegaly is a rare endocrine disorder associated with multiple complications and increased mortality. Timely diagnosis and adequate treatment can bring the life expectancy of patients with acromegaly closer to the general population level. The tests for the diagnosis of acromegaly are measurement of both serum GH, and GH after oral glucose administration; serum insulin-like growth factor-1 (IGF-1). However, in clinical practice, up to 39% of patients with discordant results are found. The patients with discordant GH and IGF-1levels, are the most difficult to manage. This review discusses the prevalence of discordant GH and IGF-1 outcomes in patients with acromegaly; factors causing this discrepancy; the impact of hormone levels on treatment outcomes. Although endocrinologists are used to dealing with this discrepancy in clinical practice for many years, discordant patients’outcome remains uncertain and undefined The optimal treatment should be individually tailored for each patient, taking into account all clinical parameters.
Carbohidrates metabolism disturbancies
Low-carb diets have been successfully used to alleviate a number of severe neurological diseases for about 100 years. The publication of the results of new studies suggesting that this type of diet may play a therapeutic role in other pathologies such as diabetes, obesity, polycystic ovary syndrome, and oncology is of particular interest for both doctors and the public. However, the long-term safety of using a low-carb or ketogenic diet, as well as its impact, primarily on the risks of developing cardiovascular diseases, remains poorly studied. This article presents the results of observation of patients against the background of a low-carbohydrate diet, both in the short-term perspective as well as provides an assessment of its long-term consequences.
Bones & Adipose tissues diseases
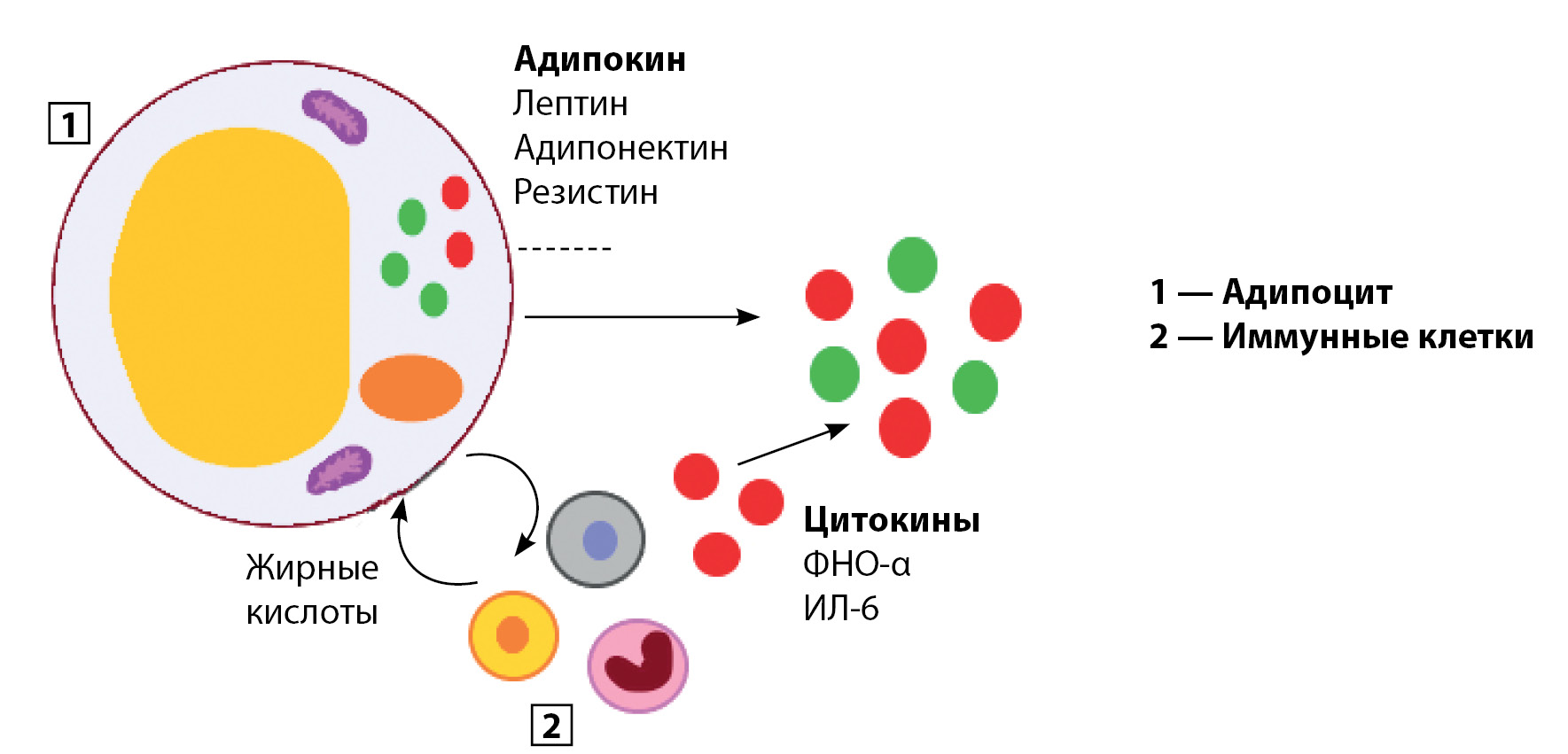
Adipose tissue is an endocrine organ which produces a large number of secretory bioactive substances also known as adipocytokines affecting directly insulin resistance (IR), glucose and lipid metabolism, angiogenesis and inflammation. The studies show a close connection between the imbalance of adipocytokines formed as a result of excessive deposit of adipose tissue in the course of the development of type 2 diabetes mellitus and cardiovascular diseases. In the present review, we summarize current data on the effect of the adipocytokines on the liver, skeletal muscles, adipose tissue, endothelial cells and inflammatory processes, as well as attempt to define the term «adipocytokines» and classify adipocytokines according to their influence on metabolic processes and pro-inflammatory status. Some of adipocytokines (adiponectin, omentin, leptin, resistin, tumor necrosis factor-α and interleukin-6) are divided into two groups: adipocytokines reducing IR, and adipocytokines increasing IR.
Multiple endocrine neoplasia type 1 syndrome (MEN1) is a rare inherited disorder that can include combinations of more than 20 endocrine and non-endocrine tumors. Unfortunately, none of the described MEN1 mutations has been associated with a peculiar clinical phenotype, even within members of the same family, thus a genotype-to-phenotype correlation does not exist. MEN1 syndrome is the most common cause of hereditary primary hyperparathyroidism (PHPT), the disease penetrance of which exceeds 50% by the age of 20 and reaches 95% by the age of 40. At the same time, PHPT with hyperplasia or adenomas of the parathyroid glands (PTG) is the most distinctive manifestation of the MEN1 syndrome. One of the main symptoms of PHPT, both in sporadic and hereditary forms of the disease, is bone damage. At the time of diagnosis in PHPT/MEN1, the bone mineral density is generally lower in comparison with the sporadic form of PHPT. This may be due to excessive secretion of parathyroid hormone during the period of peak bone mass, concomitant components of the syndrome, extended surgical treatment, and the direct effect of a mutation in the menin gene on bone remodeling. This clinical case describes a young patient with severe bone complications of PHPT and uncertain rare MEN1 mutation. PHPT was diagnosed five years later from the first onset of bone complications and repeated orthopedic operations. There was the «hungry bones» syndrome after successful surgery of PHPT, which was managed with vitamin D and calcium carbonate supplementation and there is a positive dynamic in increased bone mineral density in the main skeleton after 6 months.
Reproductive Endocrinology
BACKGROUND: Melatonin is the main hormone of the pineal gland. By regulating circadian rhythms and being an immune regulator and antioxidant, this hormone takes part in the work of the ovaries: its high concentrations block apoptosis and neutralize reactive oxygen species involved in folliculogenesis, ovulation, egg maturation and corpus luteum formation.
AIM: To study melatonin status and its relationship with menstrual dysfunction and sleep disorders in obese women of reproductive age.
MATERIALS AND METHODS. In a one-stage comparative study, women 18-35 years old took part: 30 patients with obesity and menstrual disorders of an inorganic nature and 30 healthy women in the comparison group with normal weight and regular menstrual cycle. All participants underwent a questionnaire to identify somnological disorders, and the level of melatonin in saliva and 6-sulfatoxymelatonin in urine was also investigated.
RESULTS: In the group of patients with obesity (n=30), various sleep disorders were encountered in 47% of cases (p=0.003), including more often obstructive sleep apnea syndrome was recorded (30% of cases), and a correlation was found between the indicators of the questionnaire survey of subjective sleep characteristics and body mass index of patients (r=0.450, p=0.030) compared with a group of healthy women with normal weight (n=30). In the main group, the level of melatonin in saliva was statistically significantly lower than in the control: median 12.6 pg / ml and 25.5 pg / ml, respectively (p=0.008), the same pattern was recorded for 6-sulfatoxymelatonin: 14, 72 pg / ml and 31.12 pg / ml, respectively.
CONCLUSION: Patients with obesity and menstrual dysfunction are more likely to suffer from various sleep disorders and have lower levels of melatonin in saliva and 6-sulfatoxymelatonin in urine.
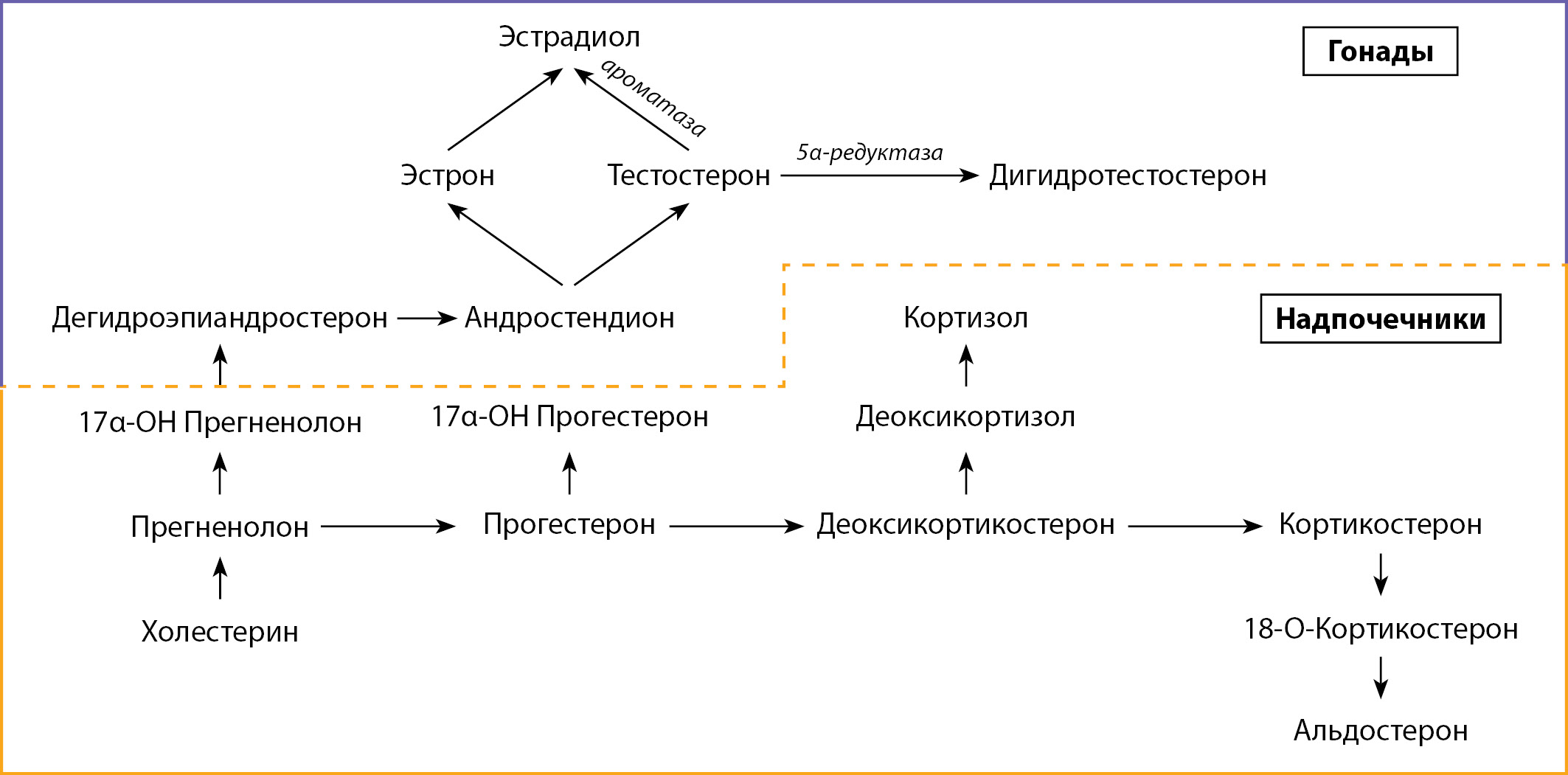
Testosterone replacement therapy (TRT) is one of the most effective and common treatments for testosterone deficiency today. It is often prescribed, focusing only on the level of testosterone and the presence of patient complaints about a decrease in sexual function. Quite rarely, doctors additionally assess the level of estradiol and, as a consequence, the initial presence of a symptom of hyperestrogenism. One of the likely consequences of the appointment of TRT may be an excess of estradiol, the excess formation of which is associated with the enzyme aromatase, which converts testosterone into estradiol. Despite the availability of laboratory determination of the level of estradiol, the result may not always coincide with the clinical picture, one of the reasons is the difference in the methods for determining the level of estradiol in each laboratory, there is no single standard or «reference» today. This article describes the evolution of TRT, and also focuses on the variability of estradiol levels from laboratory to laboratory, and explains in detail why the assessment of estradiol over time should be carried out in only one laboratory. A systematic literature search was carried out in the databases Medline, Scopus, Web of Science and Elibrary, CyberLeninka.
The purpose of our review was the need to engage the attention of specialists to the problem of hyperestrogenism, the not always justified prescription of TRT in patients with obesity, hypogonadism and hyperestrogenism, as well as to the problem of laboratory diagnosis of hyperestrogenism, which is acute not only in our country, but all over the world.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2308-1430 (Online)









































.jpg)


