Editorial notice
The article presents current data on the prevalence of thyroid diseases associated with iodine deficiency in Russia, focuses on the features of the comorbidity of iodine deficiency and autoimmune thyroid pathologies, methods for assessing the iodine supply of the population. Information about the study and prevention of iodine deficiency diseases (IDD) in the USSR and the Russian Federation is given. The history of legislative initiatives aimed at eliminating dietary iodine deficiency and preventing IDD is illustrated in detail. The ways of solving the problem of iodine deficiency at the present stage, both at the federal and regional levels, are proposed.
Oncoendocrinology
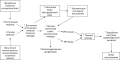
BACKGROUND: In most cases adrenal tumours are detected by accident while performing medical imaging tests for other diseases. These findings are treated as adrenal incidentaloma. Prevalence of incidentalomas detected on CT scans is up to 4%. According to different authors, 4–12% of all adrenal tumours are adrenocortical carcinomas. As for today, the most significant medical imaging technique is CT scan with bolus IV injection of contrast agent and assessment of tumour’s density. The analysis of the results of CT imaging in 67 patients with ACC was carried out according to a single protocol. The main signs characteristic of this disease are described. It is very important to evaluate typical signs of ACC on CT scans for risk assessment of ACC before surgical treatment. If malignant tumour is suspected during preoperative examination, it is extremely important to choose the right surgical treatment strategy.
AIM: To evaluate the significance of CT as the main method of preoperative diagnosis in patients with malignant tumors of the adrenal cortex. Studying CT semiotics of adrenocortical cancer in a large group of patients using a single standard imaging protocol. Find the main radiological symptoms characteristic of adrenocortical cancer
MATERIALS AND METHODS: Here are the results of retrospective study of CT scans performed on 67 patients with adrenocortical carcinoma who received treatment in the Department of Endocrine Surgery of Saint-Petersburg State University N.I. Pirogov Clinic of High Medical Technologies during 2012–2020. The diagnostic significance of CT in patients with ACC was assessed.
RESULTS: The most common features of ACC: tumour heterogeneity (84.3%), tumour’s size 3–9 cm (75%), signs of invasion into surrounding structures (10%), pre-contrast density above +30 HU (75%), absolute contrast washout less than 60% (68.8%), relative contrast washout less than 40% (64.6%)
CONCLUSION: CT scan with IV contrast was not able to show any definitive pathognomonic signs of ACC. Nevertheless, CT scan should be performed in all patients with suspected (or confirmed using other medical imaging technique) adrenal tumour according to standard protocol. Bolus injection of contrast agent should be performed in all patients with tumour’s pre-contrast density above +5 HU.
Clinical endocrinology
The frequency of chronic postoperative hypoparathyroidism after total parathyroidectomy for secondary and tertiary hyperparathyroidism in patients with end-stage renal failure, according to various authors, can reach 20% or more. Prescribing active metabolites of vitamin D and calcium it is not always sufficient for achievement of target goals. This dictates the need for replacement therapy with recombinant parathyroid hormone. Teriparatide is the only drug of this series approved by the American Food and Drug Administration (FDA) and registered in the Russian Federation. However, it is registered as an anabolic anti-osteoporotic drug and is not indicated for the treatment of chronic hypoparathyroidism. The use of teriparatide in postoperative hypoparathyroidism in patients receiving renal replacement therapy with programmed hemodialysis in the Russian Federation has not been previously studied. Data on this issue is also limited in foreign literature. However, it is a potential treatment option for hemodialysis patients with chronic hypoparathyroidism and severe bone disorders. In this article, we present 2 clinical cases of substitution and anabolic therapy with teriparatide in this cohort of patients.
Presented case demonstrates a rare diencephalic pathology — adipsic diabetes insipidus (ADI) with severe hypernatremia in a 58-year-old woman after ttranssphenoidal removal of stalk intraventricular craniopharyngioma. ADI was diagnosed because of hypernatremia (150–155 mmol/L), polyuria (up to 4 liters per day) and absence of thirst. Normalization of water-electrolyte balance occurred on the background of desmopressin therapy and sufficient hydration in postoperative period. After release from the hospital, the patient independently stopped desmopressin therapy and did not consume an adequate amount of fluid of the background of polyuria. This led to severe hypernatremia (155–160 mmol/L) and rough mental disorders.
Patients with ADI need closely monitoring of medical condition and water-electrolyte parameters, appointment of fixed doses of desmopressin and adequate hydration.
Sarcoidosis is a systemic inflammatory disease of unknown etiology characterized by the formation of noncaseating granulomas in various organs and tissues and the activation of T-cells at the site of granulomatous inflammation with the release of various chemokines and cytokines [1]. The incidence on average ranges from 10 to 20 per 100,000 population [2]. Most often in patients with sarcoidosis, lesions of the lungs and intrathoracic lymph nodes are detected. Significantly less often (in about 5–20% of patients) damage to the nervous system is noted [6,7,9]. In 9-18% of patients with neurosarcoidosis, involvement of the pituitary gland, pituitary infundibulum and hypothalamus is found, which is manifested by a variety of clinical symptoms [8,10]. We observed a patient with sarcoidosis whose disease debuted with clinical symptoms of hypogonadism, followed by the development of signs of secondary hypothyroidism, adrenal insufficiency, and diabetes insipidus, which was initially regarded as panhypopituitarism against the background of a hypothalamic lesion of unknown origin. Later, additional examination revealed signs of intrathoracic lymphadenopathy and focal changes in the lung parenchyma on CT, as well as skin lesions. Despite the biochemical compensation of hypopituitarism, the clinical efficacy of hormonal therapy with cabergoline, testosterone, hydrocortisone and levothyroxine sodium was insufficient, and the patient’s condition improved after the addition of immunosuppressive and anti-inflammatory therapy with methotrexate and methylprednisolone.
BACKGROUND: Differential diagnosis between the normocalcemic primary hyperparathyroidism (nPHPT) and secondary hyperparathyroidism (SHPT) due to hypercalciuria remains a challenge.
AIM: The aim of this study was to investigate the capability of short test with hydrochlorothiazide for the differential diagnosis of nPHPT and SHPT.
MATERIALS AND METHODS: A retrospective study was conducted with the participation of 28 patients who underwent a functional test with thiazide diuretics during hospitalization in the Department of parathyroid glands pathology and mineral disorders of the Endocrinology Research Centre, Russia. Parameters of mineral metabolism were evaluated before and 3–5 days after taking hydrochlorothiazide 50 mg/day.
RESULTS: According to baseline and dynamic biochemical evaluation patients were divided into 3 groups. Group 1 (n=21) included patients with confirmed PHPT, who reached hypercalcemia accompanying with an elevated level of iPTH (n=19) or an increased level of iPTH accompanying with normocalcemia (n=2). In group 1, baseline Caadj. was 2.48 mmol/l [2.47; 2.52], iPTH 107.5 pg/ml [86.8; 133.0], after short test — 2.63 mmol/l [2.59; 2.66] and 102.1 pg/ml [95,7; 124,1]. Group 2 included only one who was diagnosed with SHPT, a normal value of iPTH with concomitant normocalcemia was achieved after 4 days of hydrochlorothiazide therapy (baseline Caadj. 2.35 mmol/l, iPTH 74.5 pg/ml vs at 2.27 mmol/l and 50.7 pg/ml respectively). Patients with doubtful results of the test entered in group 3 (n=6), they did not achieve significant changes in the calcium and iPTH levels, so it was recommended to continue the test on an outpatient basis (baseline Caadj. 2.39 mmol/l [2.33;2.45], iPTH 97.0 pg/ml [83.1;117.0]); after short test — 2.47 mmol/l [2.42; 2.48] and 91.3 pg/ml [86.9; 124.0] respectively). Groups with PHPT and SHPT and doubtful results significantly differed from each other in Caadj (р=0.003, U-test, Bonferroni correction Р0=0.006), but not in iPTH, daily calciuria, eGFR, and phosphorus. There were no significant differences in the incidence of classical complications of PHPT.
CONCLUSION: The diagnosis of PHPT was confirmed in 21/28 patients 3–5 days after taking hydrochlorothiazide 50 mg/day. The obtained results are significant for the differential diagnosis in hospitalized patients with an unspecified genesis of hyperparathyroidism.
Carbohidrates metabolism disturbancies
BACKGROUND: Insulin resistance (IR) is the root cause of most age-related diseases (ARD), the major challenge for today’s health systems. Therefore, adequate understanding of the mechanisms underlying IR is essential to build effective ARD prevention.
OBJECTIVE: Analyze the existing models of IR causation and progression in order to justify the most effective ARD prevention strategy.
METHODS: Search and analysis of publications on IR and hyperinsulinemia (HI) from databases elibrary.ru, PubMed, and Google Scholar.
RESULTS: Two models of IR development are analyzed along with the relationship between IR, HI, and obesity. The prevailing model considers obesity (imbalance of caloric intake and energy expenditure) as the main factor in the development of IR; HI is seen as a consequence of IR, mostly insignificant for the outcomes of IR. The model contradicts many experimental and clinical findings. The strategy to combat ARDs that follows from the model (hypocaloric diet and pharmacotherapy of IR) has proven mostly ineffective.
The alternative model (IR as a consequence of HI, and obesity as one of IR manifestations) is more consistent with the pool of experimental and clinical data. It more precisely predicts ARD development and allows more adequate correction of adverse lifestyle factors. It corresponds to a different strategy for combating ARD: emphasis on low-carb diet and longer fasting window combined with consideration of other factors of IR.
CONCLUSION: If the prevailing model of IR development is revised, this should open up opportunities for more effective early prevention of a wide range of chronic diseases in which the role of IR is significant.
The risk of cardiovascular disease (CVD) in persons with type 2 diabetes mellitus (DM2) increases two to four times. One of the main factors increasing cardiovascular risk is dyslipidemia, which includes abnormalities in all lipoproteins, including high-density lipoproteins (HDL). The development of DM2 is accompanied not only by a decrease in the level of HDL, but also by significant changes in their structure. This leads to the transformation of native HDL into so-called dysfunctional or diabetic HDL, which loses their antiatherogenic, cardioprotective, anti-inflammatory and anti-diabetic properties. In poorly controlled diabetes mellitus HDL can not only lose its beneficial functions, but also acquire proatherogenic, proinflammatory ones. Diabetic HDL can contribute to the accumulation of such unfavorable qualities as increased proliferation, migration, and invasion of cancer cells. Given that HDL, in addition to participation in cholesterol transport, performs important regulatory functions in the body, there is reason to assume that structural modifications of HDL (oxidation, glycation, triglyceride enrichment, loss of HDL-associated enzymes, etc.) are one of the causes of vascular complications of diabetes.
Bones & Adipose tissues diseases
The article provides a review of the current literature about time-restricted eating (TRE) as a new tool for the treatment of obesity and comorbid conditions. The search for new nutritional strategies in obesity, one of which is TRE, is due to the weak adherence of patients to hypocaloric diets in the long term, as well as the available data on the importance of desynchronization of food intake with natural circadian rhythms in the development and progression of obesity and cardio-metabolic complications. The article describes the main mechanisms that regulate the circadian rhythms of food intake and nutrient absorption, substantiates the importance of adhering to a physiological diet for maintaining metabolic health. The main part of the review is devoted to reviewing the currently available researches on the effectiveness of various strategies of intermittent energy restriction for weight loss and the correction of metabolic parameters. Potential mechanisms of the effect of TRE on health are discussed, including those mediated by an unintentional decrease in caloric intake and changes in eating behavior, and differences in the effectiveness of early and late TRE. The article contains a detailed discussion of the potential problems and contradictions associated with the use of time-restricted eating in clinical practice, namely: the limitations and inconsistencies of the available clinical trials, the lack of data on long-term efficacy and safety, social and psychological limitations that impede the widespread use of TRE.
Pediatric Endocrinology
Itsenko–Cushing’s disease is a rare, multisystem disease characterized by the presence of endogenous central hypercortisolism due to an ACTH-secreting brain tumor. The frequency of Itsenko-Cushing’s disease in adulthood is 0.7–2.4 per 1 million population, and only 10% of all cases occur in childhood. The age of onset of the disease in children is on average 12.0–14.8 years. A typical manifestation of the disease in children, along with obesity and arterial hypertension, is a decrease in growth rates. The gold standard for diagnosing central hypercortisolism is MRI of the brain, however, the effectiveness of this method in children is only 50%. The main method of treatment is neurosurgical transnasal transsphenoidal removal of endosellar pituitary adenoma, which makes it possible to achieve remission in more than 65% of cases. This article describes a clinical case of Itsenko–Cushing’s disease in a 6.5-year-old child with obesity, arterial hypertension, atypically «high» stature, average velocity and non-visualizable corticotropinoma. The article presents the stages of diagnostic search, the complexity of differential diagnosis and surgical treatment, the results of follow-up after the treatment and a brief review of the literature.
BACKGROUND: Myokines are synthesized by myocytes and released into the bloodstream in response to muscle fiber contraction. They have a positive effect on carbohydrate and lipid metabolism, muscle mass growth, osteogenesis, increase tissue sensitivity to insulin, counteract inflammation of adipose tissue. The study of their secretion in response to physical activity (FA) can help to personalize the therapy of obesity.
AIM: to study the features of the secretion of myokines in children with constitutionally exogenous obesity during physical activity of different duration and intensity and to evaluate their relationship with the parameters of the body composition.
MATERIALS AND METHODS: 26 children (10 boys and 16 girls) were included in the study 15 [13; 16] years old, SDS BMI: +2.91 [2.24; 3.29], with sexual development according to Tanner 4–5. Two groups of 13 people were formed by random distribution. Group I performed FA (walking on a treadmill under the control of heart rate) of different duration: 30 and 60 minutes at the same intensity (less than 3 metabolic equivalents (MET)). Group II — FA of different intensity: low — less than 3 METH and moderate — 3–6 METH with the same duration of 45 minutes. Commercial kits for enzyme immunoassay were used to determine the level of myokines. The assessment of the compositional composition of the body was carried out by bioimpedance analysis (analyzer In Body 770, South Korea) in the morning, on an empty stomach. Statistical processing was carried out using STATISTICA v.12.0 (StatSoftInc., USA). The results are presented in the form of median (Me) and quartiles (Q1; Q3) corresponding to 25 and 75 percentiles. The critical significance level (p) was assumed to be <0.05.
RESULTS: moderate intensity FA leads to a maximum increase in the level of myokines: interleukin-6 (IL-6) by 215.7% and decorin by 34.3%, a decrease in the level of irisin by 16.5%. An hour-long low-intensity workout leads to a moderate increase in the level of IL-6 by 80.5%, to a decrease in the level of irisin by 31.1%. Myostatin increases equally both after 60-minute FA and after moderate intensity FA by 30.9% and 31.8%, respectively. Short low-intensity FA (lasting 30 minutes) it is not accompanied by a significant increase in the expression of myokines. The relationship between the amount of muscle (r=0.65), lean (r=0.62), fat-free mass (r=0.64) and the level of decorin after FA was noted. There was no statistically significant relationship between the parameters of the body composition and the levels of IL-6, myostatin, and irisin. There were no gender differences in both basal and stimulated myokine secretion.
CONCLUSION: Moderate intensity FA and low intensity 60-minute FA are most effective for obese children. A 30-minute low-intensity FN is insufficient to increase the secretion of myokines by skeletal muscles.
Reproductive Endocrinology
BACKGROUND. COVID-19 is a disease that has a negative systemic effect on the human body, including the male gonads. Therefore, the androgenic status in men with COVID-19 needs to be studied.
AIM. To evaluate the levels of total testosterone, sex hormone binding globulin (SHBG) and free testosterone in men in the acute phase of COVID-19 and during convalescence.
MATERIALS AND METHODS. A continuous dynamic prospective study of 70 men with moderate to severe COVID-19 at the age of 50[44; 64] years. During the study, the levels of total testosterone, SHBG were determined with further calculation of the level of free testosterone by Vermeullen. The data were collected twice — at the patient’s hospitalization and at his discharge. The differences between the groups were considered statistically significant at p <0.05.
RESULTS. At the time of hospitalization for COVID-19, hypogonadism syndrome was observed in 61 people — 87%. Patients with hypogonadism did not statistically significant differ in age and severity of COVID-19 disease compared to men without hypogonadism. Inpatient treatment lasting 12[10;14] days resulted in a statistically significant increase in the levels of total testosterone from 4,7[2,96;8,48] to 12,85[8,62;19,2] nmol/l, p<0,001; SHBG from 27,87[20,78;36,57] to 33,76[26,27;52,60] nmol/l, p<0,001 and free testosterone from 107[65;174] to 235[162;337] pmol/l, p<0,001. This led to the elimination of hypogonadism in 28 patients — 40%. Patients with persistent hypogonadism were statistically significantly older than men with normalized testosterone, there were no statistically significant differences in the initial levels of total testosterone, SHBG and free testosterone, and there were also no differences in the prevalence of severe COVID-19 (3,97[2,86;7,46] vs 4,26[2,93;5,96] nmol/l, p=0,100; 28,76[20,78;48,59] vs 24,63[18,85;31,70] nmol/l, р=0,994; 100[58;118] vs 96[64;143] pmol/l, p=0,522; 24 vs 18%, p=0,754, respectively).
CONCLUSION. COVID-19 has a pronounced negative effect on the production of testosterone in men, leading to the development of laboratoric hypogonadism, which is potentially reversible. The reversibility of laboratoric hypogonadism is typical for younger patients.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2308-1430 (Online)












































.jpg)


