Editorial notice
The article provides brief data on the prevalence of endocrine diseases in children in the Russian Federation, provides the main normative documents regulating the provision of medical care in the field of «pediatric endocrinology», data on the state of the bed fund (children's endocrinological beds), the number of specialized children's departments in the Russian Federation, the number of children's endocrinologists.
Clinical endocrinology
BACKGRAUND: Currently high frequency of thyroid or parathyroid surgery is associated with significant increased incidence of hypoparathyroidism. Evaluation of the epidemiological and clinical features of chronic hypoparathyroidism is necessary to predict social-significant complications and to improve the quality of medical care.
AIMS: To estimate clinical and demographic features, different regimens and efficacy of conventional therapy in patients with chronic postsurgical and nonsurgical hypoparathyroidism.
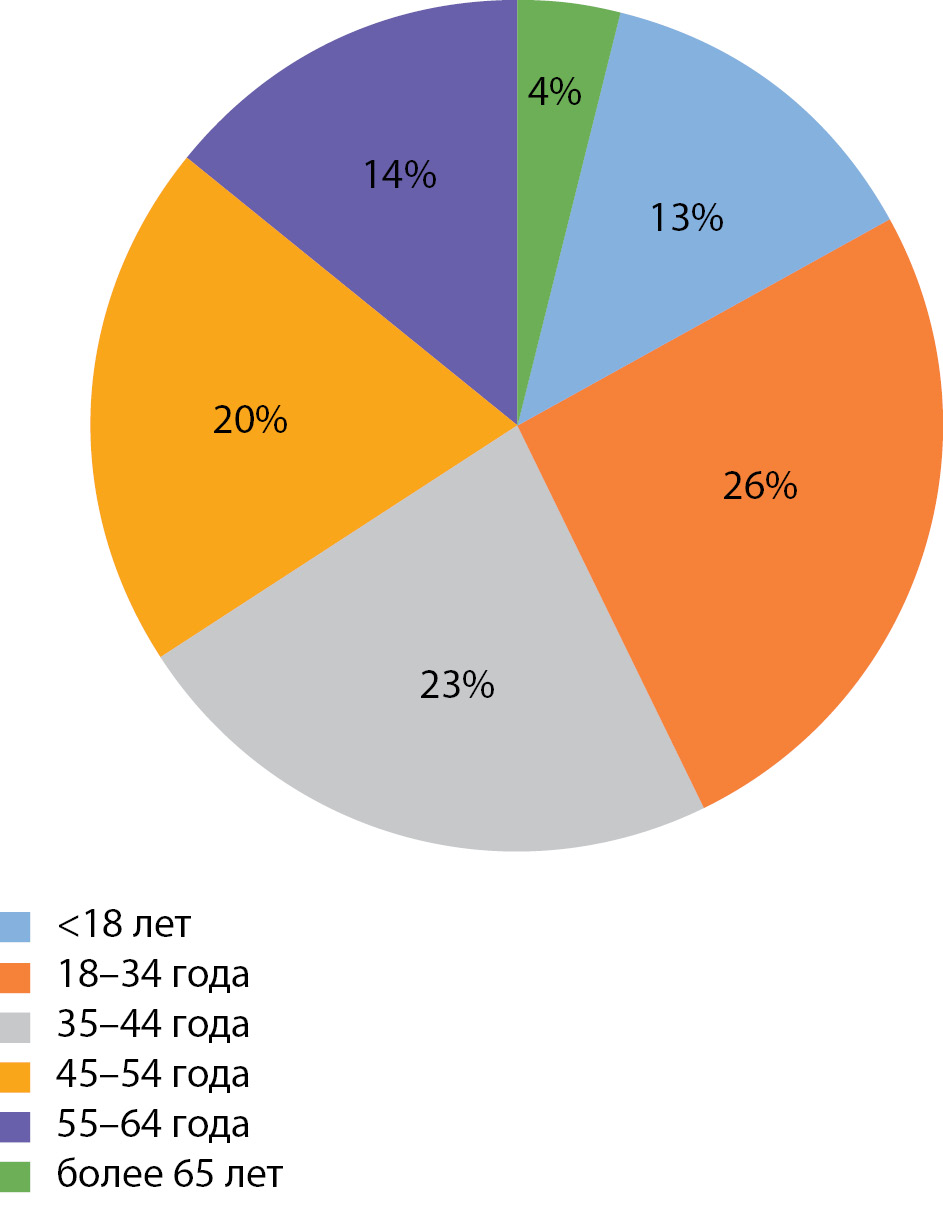
MATERIALS AND METHODS: The cross-sectional, observational, continuous study was carried out based on Database of patients with chronic postsurgical and nonsurgical hypoparathyroidism of Endocrinology Research Centre, Moscow. 293 patients from 61 regions of the Russian Federation were included in this study. Statistical analysis was done on June 2020. The descriptive statistics are presented by medians (Ме) and the first and third quartiles (Q1; Q3) and by absolute and relative frequencies.
RESULTS: Hypoparathyroidism was most often recorded in women (85%) at the age of 43 [32; 52] years, after thyroid surgery. Less than a half of the study group had target indicators of serum calcium and phosphate levels (31% and 47%, respectively) despite ongoing treatment. A complex instrumental examination for the disease complications was performed in 58% of cases (n = 169). Among them, kidney disorders were detected in 38%, visual disturbance in 14%, brain calcification in 10%, arrhythmias in 4% and neuropsychiatric symptoms in 6%. Conventional therapy with calcium supplements and activated vitamin D analogues was noted in 75% of patients.
CONCLUSIONS: The analysis of large databases of patients with chronic hypoparathyroidism is a necessary tool for determining of optimal clinical and therapeutic approaches, as well as prognostic markers of disease complications.
BACKGROUND: Graves' Orbitopathy (GO) — also known as Thyroid Eye Disease (TED) — is an autoimmune condition in the modern sense. It is closely associated with autoimmune thyroid diseases. Cytokine-mediated mechanisms play a critical part in immunopathogenesis of autoimmune thyroid diseases including GO. Investigating cytokine profiles as well as antibodies to tissue-specific antigens is essential for explaining GO pathogenesis and developing future therapeutic strategies.
AIMS: The study examines serum levels of cytokines, autoantibodies and immunoglobulins IgG and IgG4 as mediators of autoimmune inflammation in patients with GO and Graves' Disease (GD).
MATERIALS AND METHODS: The study included 52 patients (104 orbits) aged 25-70 years (mean age 48,8±12,3) in the active phase of GO and GD verified with the international diagnostic standards. These patients did not get any treatment for GO before. The control group consisted of 14 individuals (28 orbits) aged 30-68 years without known autoimmune disease.
Serum levels of IgG, IgG4,TNFα, IL-1α, IL-1β, IL-2, IL-4, IL-6, IL-8, IL-10, IL-17A, IL-13, sIL-6R, sTNFα- RI и TNFα- R2 IL-2R, TGFβ1, TGF β3, antibodies to TSH-receptor, free T4, free T3 and TSH were measured. A diagnostic ultrasound exam of thyroid gland, multislice computed tomography (MSCT) / magnetic resonance imaging (MRI) of orbits were performed.
RESULTS: Mean duration of GO prior to being admitted to the centre was 8,8±1,5 months (range: 1 — 48 months). According to the degree of thyrotoxicosis compensation: 24 patients were clinically euthyroid, TSH 3,3±0,7 mU/L, free T4 11,9±0,59 pmol/L, free T3 3,97±0,1 pmol/L; 28 patients were considered to have subclinical thyrotoxicosis: TSH 0,03±0,01 mU/L, free T4 14,2±1,0 pmol/L, free T3 5,77±0,49 pmol/L. Serum levels of sTNFα-R2 (p=0,041, p≤0,05), sIL-2R (p=0,020, p≤0,05), TGFβ1 (p=0,000, p≤0,001) were significantly higher in patients with GO compared to the control group. Serum levels of sTNFRα2 (p=0,038, p<0,05) and TGFβ1 (P=0,011, p≤0,05) were positively correlated with the duration of GO. The positive correlations between the serum level of sIL-6R (p=0,034, p≤0,05) and the severity of GO as well as between the serum level of sTNFα- R 1 (P=0,012, p≤0,05) and activity of GO were observed. 54% of patients had elevated concentration level of IgG4 in IgG ( >5%).
CONCLUSION: High levels of soluble cytokine receptors sTNFα-R2 and sIL-2R and cytokine TGFβ1 in patients with long-standing untreated GO and GD being euthyroid or having subclinical thyrotoxicosis indicate activation of regulatory T cells aimed at suppressing autoimmune processes. High concentration level of IgG4 in IgG and cytokine TGFβ1 can determine the development of fibrotic changes in the orbital tissues. A decrease in the concentration of cytokine TGFβ1 can indicate an unfavorable course of the disease GO.
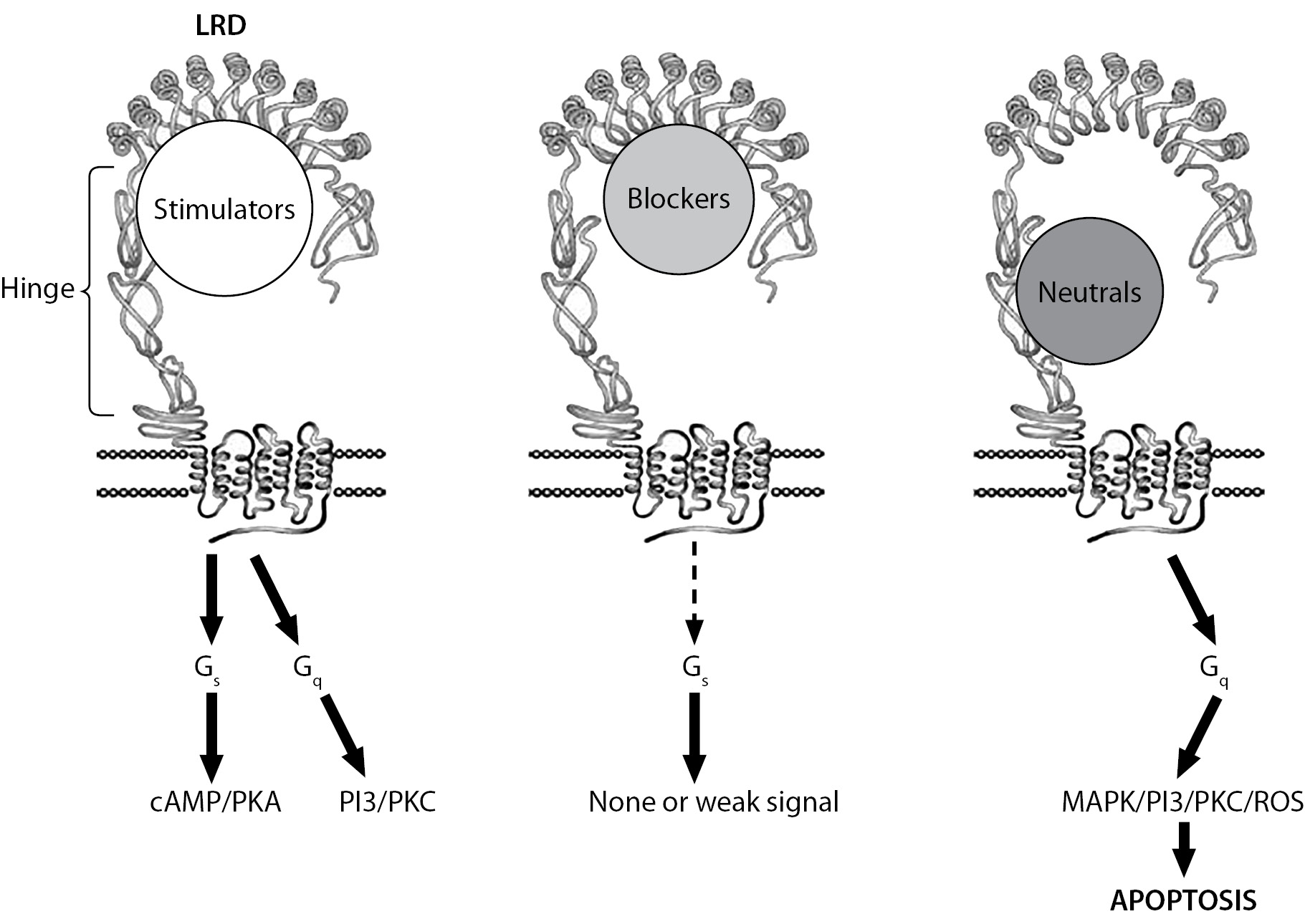
The main autoimmune thyroid diseases are Hashimoto's thyroiditis (HT) and Graves' disease (GD). Despite the significant differences in a pathogenesis and a clinical picture between HT and GD, the literature describes the cases of the conversion of one autoimmune disease to another, which, according to one version, is associated with a change in the balance between the levels of a stimulating and blocking antibodies to the thyroid-stimulating hormone receptor. At the same time, there are more frequent observations of the transition of GD to HT, and much less often describe, on the contrary, the development of GD against the background of HT. The article presents a clinical case of the conversion of HT to GD. A detailed algorithm of the conservative management according to the «block-replace» scheme is described, indicating the results of laboratory and instrumental examination. At the time of describing the clinical case, the result of the treatment can be considered successful. The predictors such as a low level of the thyroid-stimulating hormone receptor and thyroid volume before discontinuation of the thyrostatic therapy suggest a low risk of the recrudescence of GD.
According to the authors, the phenomenon of the conversion of one autoimmune thyroid disease to another, in addition to the scientific interest, is important for the practitioners, since a timely change in the diagnostic paradigm can significantly change the treatment strategy and the favorably affect the prognosis of disease, preventing the development of complications.
Bones & Adipose tissues diseases
BACKGROUND: Quercetin (Q; 3,3',4',5,7 - pentahydroxyflavone) can help alleviate the pathological effects of nutritional obesity and metabolic syndrome when taken as part of products for special dietary needs and food supplements. The mechanisms of action of Q at the genetic level are not well understood.
AIMS: To study gene expression in liver tissue of mice with alimentary and genetically determined obesity upon intake of Q with diet.
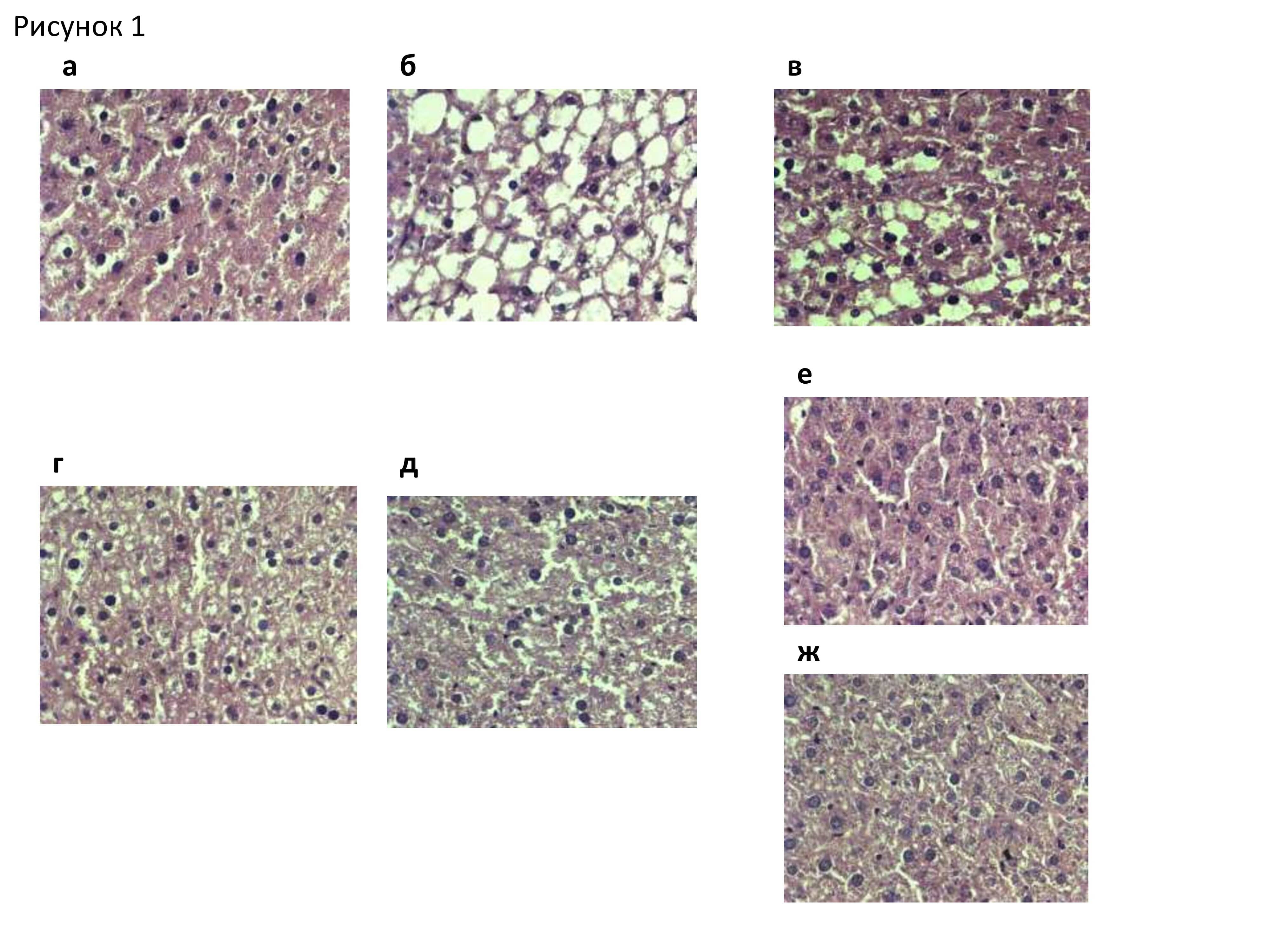
MATERIALS AND METHODS: During 46 days of the experiment on 32 male C57Bl/6J mice fed a diet with an excess of fat and fructose and 24 male genetically obese db/db mice the effect of Q in dose of 25 or 100 mg/kg of body weight was studied on differential expression of 39430 genes in mice livers by full transcriptome profiling on microchip according to the Agilent One-Color Microarray-Based Gene Expression Analysis Low Input Quick Amp Labeling protocol (version 6.8). To identify metabolic pathways (KEGGs) that were targets of Q exposure, transcriptomic data were analyzed using bioinformatics methods in an “R” environment.
RESULTS: Differences were revealed in the nature of Q supplementation action in animals with dietary induced and genetically determined obesity on a number of key metabolic pathways, including the metabolism of lipids and steroids (Saa3, Cidec, Scd1, Apoa4, Acss2, Fabp5, Car3, Acacb, Insig2 genes), amino acids and nitrogen bases (Ngef, Gls2), carbohydrates (G6pdx, Pdk4), regulation of cell growth, apoptosis and proliferation (Btg3, Cgref1, Fst, Nrep Tuba8), neurotransmission (Grin2d, Camk2b), immune system reactions (CD14i, Jchain, Ifi27l2b).
CONCLUSIONS: The data obtained help to explain the ambiguous effectiveness of Q, like other polyphenols, in the dietary treatment of various forms of obesity in humans, as well as to form a set of sensitive biomarkers that allow us to elucidate the effectiveness of minor biologically active food substances in preclinical trials of new means of metabolic correction of obesity and metabolic syndrome.
BACKGROUND: Pathological low-energy (LE) vertebral compression fractures (VFs) are common complications of osteoporosis and predictors of subsequent LE fractures. In 84% of cases, VFs are not reported on chest CT (CCT), which calls for the development of an artificial intelligence-based (AI) assistant that would help radiology specialists to improve the diagnosis of osteoporosis complications and prevent new LE fractures.
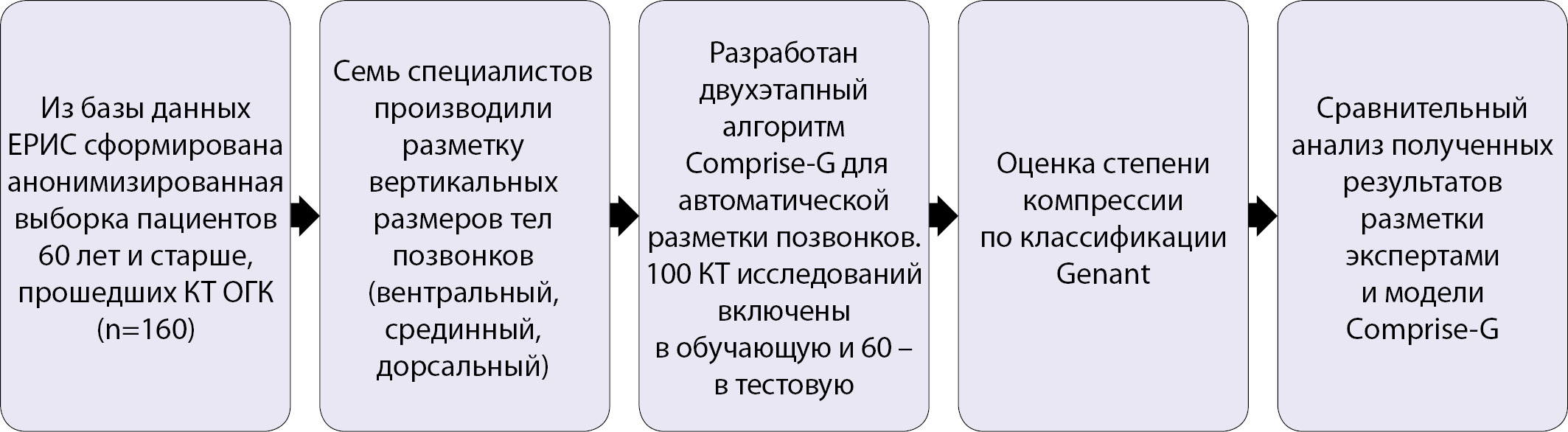
AIMS: To develop an AI model for automated diagnosis of compression fractures of the thoracic spine based on chest CT images.
MATERIALS AND METHODS: Between September 2019 and May 2020 the authors performed a retrospective sampling study of ССТ images. The 160 of results were selected and anonymized. The data was labeled by seven readers. Using the morphometric analysis, the investigators received the following metric data: ventral, medial and dorsal dimensions. This was followed by a semiquantitative assessment of VFs degree. The data was used to develop the Comprise-G AI mode based on CNN, which subsequently measured the size of the vertebral bodies and then calculates the compression degree. The model was evaluated with the ROC curve analysis and by calculating sensitivity and specificity values.
RESULTS: Formed data consist of 160 patients (a training group - 100 patients; a test group - 60 patients). The total of 2,066 vertebrae was annotated. When detecting Grade 2 and 3 maximum VFs in patients the Comprise-G model demonstrated sensitivity - 90,7%, specificity - 90,7%, AUC ROC - 0.974 on the 5-FOLD cross-validation data of the training dataset; on the test data - sensitivity - 83,2%, specificity - 90,0%, AUC ROC - 0.956; in vertebrae demonstrated sensitivity - 91,5%, specificity - 95,2%, AUC ROC - 0.981 on the cross-validation data; for the test data sensitivity - 79,3%, specificity - 98,7%, AUC ROC - 0.978.
CONCLUSIONS: The Comprise-G model demonstrated high diagnostic capabilities in detecting the VFs on CCT images and can be recommended for further validation.
Familial hypocalciuric hypercalcemia (FHH) - rare disease with predominantly autosomal dominant inheritance. FHH typically develops due to a heterozygous inactivating mutation in the calcium-sensitive receptor gene (CASR), less commonly due to heterozygous mutations in GNA11 and AP2S1. CASR mutations lead to an increase in the threshold for calcium sensitivity, which requires a higher concentration in serum to reduce the release of PTH. These changes are accompanied by an increase of calcium and magnesium reabsorption in the proximal tubules, which leads to hypercalcemia and hypocalciuria. Basically, FHH may be asymptomatic or accompanied by mild hypercalcemia. FHH doesn't require surgical treatment, unlike primary hyperparathyroidism (PHPT), therefore, differential diagnosis of these two conditions is extremely important. In addition, immediate relatives of a proband with FHH also require the exclusion of disease inheritance. We analyzed a series of clinical cases with a genetically confirmed diagnosis of FHH. Our clinical cases indicate a variety of clinical manifestations and the difficulties of differential diagnosis with PHPT.
Pediatric Endocrinology
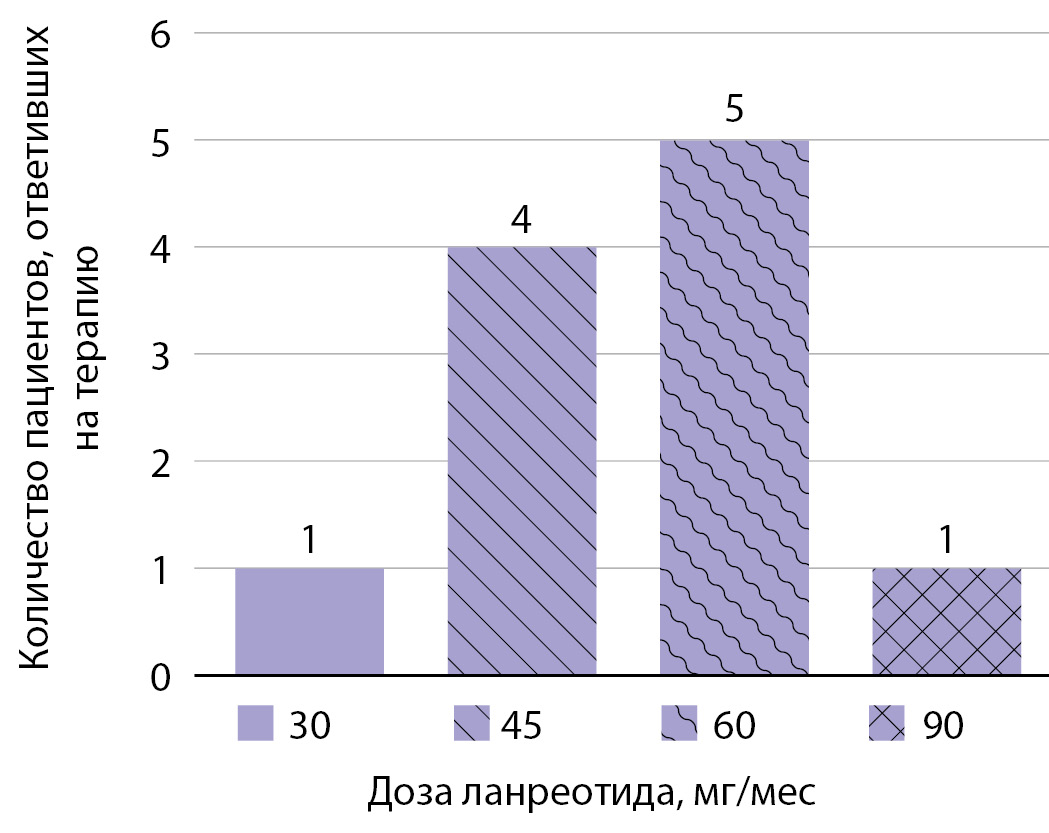
BACKGROUND: Children with congenital hyperinsulinism (CHI), a severe orphan disease, are still one of the most demanding patients in the endocrinology practice. The use of first- and second-line drugs is not always effective and has a number of restrictions. Lanreotide — long-acting somatostatin — represents an alternative insulinostatic therapy. The main advantage of lanreotide is stable concentration of the drug in the blood that enables minimizing the number of injections. However, the experience of using lanreotide in the treatment of CHI is limited to small groups of patients. There is also a problem of the absence of a standardized regimen in clinical practice; and the calculator for evaluating the initial effective drug dose is needed.
AIM of the study is to evaluate the effectiveness and safety of lanreotide therapy in the treatment of CHI in children.
MATERIALS AND METHODS: An open single-center observational study was conducted on the basis of Endocrinology Research Centre. The study included diazoxide-unresponsive pediatric patients with CHI who were initially treated with octreotide in different modes: multiple daily subcutaneous injections or continuous subcutaneous infusion via pumps. The indicators of the effectiveness and safety of the lanreotide therapy were evaluated shortly after the first injection and lately on a regular visit after further injections.
RESULTS: The study group included 12 patients. Persistent euglycaemia was achieved in 67% of the subjects (8/12). Complete effectiveness of the therapy was observed in 8/12 patients (67%), partial — in 3/12 (25%), and lack of effectiveness — in 1/12 of the patient (8%). The age of the patients at the time of lanreotide administration was 6 months (5; 15). According to the study, the most effective dose of lanreotide is 3.5-5.5 mg/ kg/ month. There were no significant side effects observed.
CONCLUSIONS: The use of lanreotide in patients with diazoxide-resistant congenital hyperinsulinism was effective and safe in the vast majority of the patients. Moreover, we were able to calculate the effective dosage of lanreotide in CHI patients which fulfilled the clinical demand.
Differential diagnosis of hypoglycemic syndrome remains an urgent problem in Pediatrics. In this article, a case of glycogen storage disease (BNG) type 0 is described in the boy, which is undoubtedly a rare pathology, which makes it difficult to diagnose this form of glycogenosis. In this description, the case of type 0 BNG is caused by a mutation in the GYS2 gene encoding the hepatic isoform of glycogen synthase. This form of the disease is usually asymptomatic in infancy. However, it can be suspected in the case when the refusal of night feeding causes certain difficulties due to the hungry ketotic hypoglycemia that occurs in the child. The first clinical symptoms appear in early childhood with the inclusion of a more varied diet in the child, increasing the intervals between meals. Symptoms of the disease are primarily caused by hypoglycemia. It should be noted that, despite the low levels of glycemia, most children do not have any mental development disorders, since the increase in the level of ketone bodies in the blood plasma provides the brain with an alternative source of energy.
Carbohidrates metabolism disturbancies
BACKGROUND: The prevalence of T2DM is steadily increasing not only among the elderly, but also at a young age. T2DM is preceded by a long period of significant metabolic changes with the development of insulin resistance and в-cell dysfunction. To reduce the prevalence of complications, treatment is needed which affects several pathophysiological mechanisms underlying the disease. Monotherapy with metformin at the onset of T2DM is often insufficient. The VERIFY study demonstrated the advantage of early administration of a combination of vildagliptin and metformin in relation to the glycemic durability compared to the sequential intensification of metformin with vildagliptin in patients with type 2 diabetes.
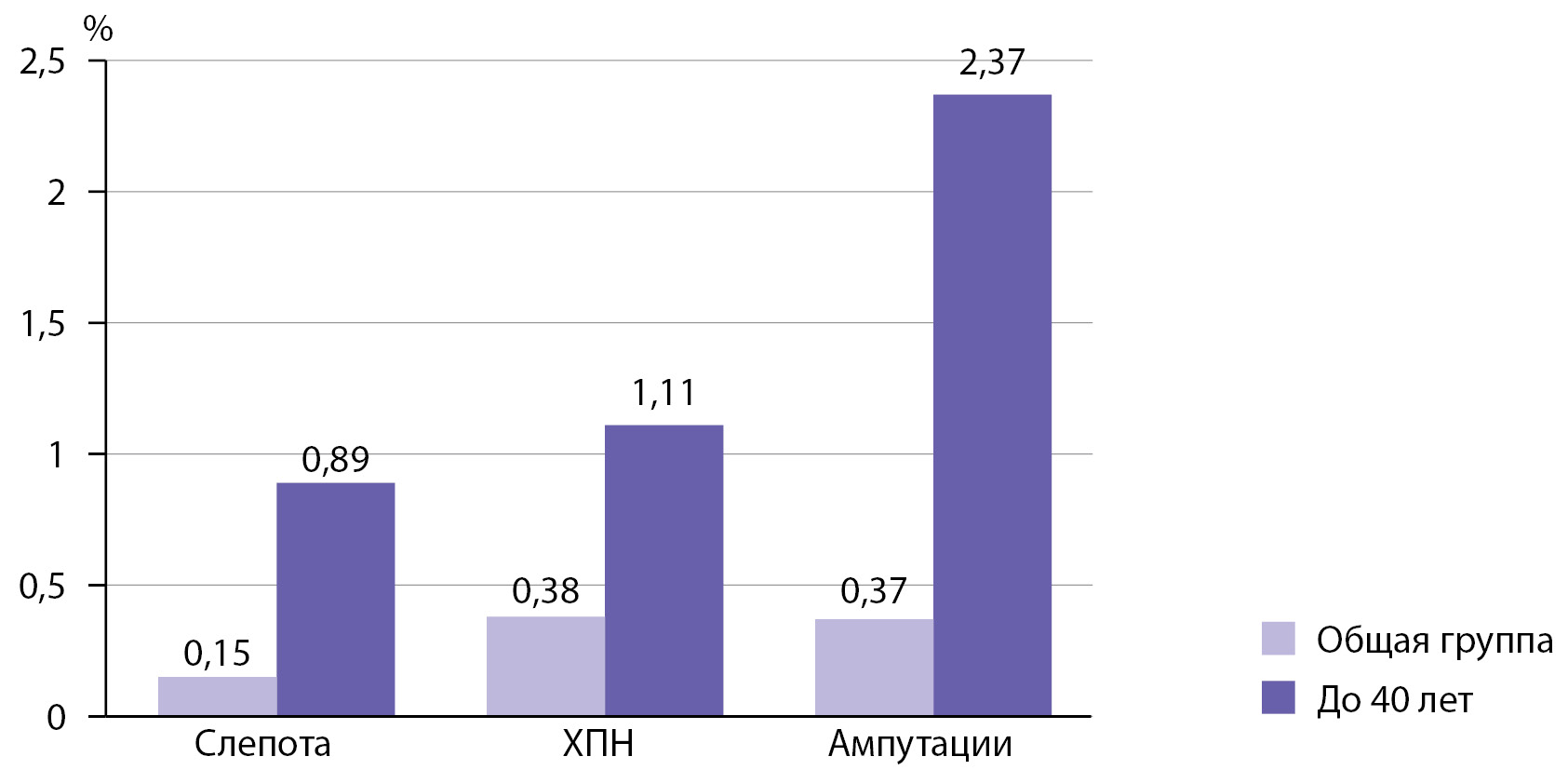
AIMS: To assess the current situation in terms of the incidence of T2DM complications and the structure of the prescribing glucose lowering drugs based on the data from the Diabetes Register (DR) of the Moscow Region. To demonstrate the advantages of early combination therapy in patients with newly diagnosed T2DM using clinical cases.
MATERIALS AND METHODS: The data from the DR of the Moscow region, which is part of the National Diabetes Register of the Russian Federation, were used for the analysis. The data of 6,096 patients with T2DM who died in 2019 were evaluated for building the structure of the causes of death of patients with T2DM. The pattern of glucose-lowering therapy was analyzed based on data of 226,327 patients with T2DM (for 2020), as well as separately of 14,379 patients with newly diagnosed T2DM in 2019. Clinical cases are described based on the data of two patients with T2DM, available in the DR database and outpatient records.
RESULTS: In patients with young onset T2DM (<40 years), the prevalence of severe complications is higher than in the general population of patients with T2DM: blindness is in 5.9 times, end-stage chronic renal failure in 2.9 times, lower limb amputations in 6.4 times more. When prescribing glucose lowering drugs, monotherapy is prevalent, mostly metformin. In double combination, metformin is used in 96.22% of cases. In the structure of glucose lowering drugs, with newly diagnosed T2DM, combination therapy is used less frequently than in patients with T2DM in general. Of the drugs of the IDP-4 group, vildagliptin is most often prescribed — 46.25% (including of a fixed combination with metformin — 12.22%). Clinical cases reflect a rapid clinical outcome: a decrease in HbA1c to the target in 6 months, the absence of hypoglycemia or other side effects, and positive weight dynamics.
CONCLUSIONS: A fairly large propotion of patients with T2DM are on monotherapy with glucouse lowering drugs. Early prescription of the combination of metformin plus vildagliptin provides a longer maintenance of glycemic control without increasing the risk of hypoglycemia and weight gain for patients with newly diagnosed T2DM.
Reproductive Endocrinology
Vitamin D insufficiency and deficiency in women with infertility is more common than in the population. However, we still do not know the exact mechanisms for the participation of vitamin D in the regulation of reproductive function. The purpose of this study is to analyze actual literature data on the role of vitamin D in the regulation of reproductive system and its influence on using of assisted reproductive technologies for the treatment of infertility. A search was carried out for literary sources published in the NSBI database PubMed, Medline, and others with a search depth of up to 20 years. 135 sources on this topic were studied, of which 54 were included in the analysis. The review presents data obtained in animal studies, in vitro and in clinical studies. Thus, the absence of vitamin D resulted in a dramatical decrease in fertility in both female and male rats and mice, due to the development of hypocalcemia. In vitro studies describe its involvement in the receptive transformation of the endometrium and in the regulation of the immune response during embryo implantation. However, clinical studies often show conflicting results. There is no unequivocal data on the effect of vitamin D levels on spermogram parameters, but a decrease in the pregnancy rate was shown when ovulation was induced in pairs, where a vitamin D deficiency was revealed in men. A meta-analysis published in 2017 showed a decrease in the pregnancy and live birth rate in women with low levels of vitamin D after the use of assisted reproductive technologies (ART). It was not possible to establish whether this decrease depends on oocyte quality or endometrium. There is an opportunity that the effect of vitamin D deficiency on fertility will not come with all forms of infertility. For example, in women with anovulation due to polycystic ovary syndrome, vitamin D deficiency is demonstrated to decrease pregnancy rate in ovulation induction cycles and in ART. Such relationship was not found in women with unexplained infertility.
Thus, the role of vitamin D in the pathogenesis of infertility requires further study, as well as the possibilities of therapy in order to increase the effectiveness of infertility treatment methods and assisted reproductive technology programs.
ISSN 2308-1430 (Online)









































.jpg)


