Editorial notice
BACKGROUND: The cocaine-amphetamine regulated transcript has been discovered long time ago (circa over 25 years ago) but still stays not enough investigated. Just during last five years scientist’s society started providing interest to the genomic, proteomic and metabolic essence of the cocaine-amphetamine regulated transcript.
AIM: The evaluation of historical pathway and perspectives of the cocaine-amphetamine regulated transcript medical investigations.
MATERIALS AND METHODS: The literature search has been provided via Russian (eLibrary, CyberLeninka.ru) and international (PubMed, Cochrane Library) databases and among articles on Russian and English languages. The main criteria for article selection was free access and 2019–2021 years of publishing. Although the introduction is based on the articles published in 1989. The present article was created according to the federal project «Central and peripheral pathophysiological mechanisms of adipose tissue diseases and their clinical and hormonal manifestations» (2020–2022)
RESULTS AND CONCLUISON: It is necessary to keep on investigating genomic, proteomic and metabolomic markers because they contain important clues for successful resistance against human diseases. The 21st century is the era of transformation from simple clinical medicine to personalized science. For example, researches in the area of cocaine-amphetamine regulated transcript may result in invention of genetic medicine against dangerous metabolic diseases.
Clinical endocrinology
Primary hyperaldosteronism (PHA) is the most common form of endocrine hypertension. Until recently, the reason for the development of this condition was believed to be the presence of genetic mutations, however, many studies declare that the disease can be polyetiologic, be the result of genetic mutations and autoimmune triggers or cell clusters of aldosterone-producing cells diffusely located in the adrenal gland at the zona glonerulosa, zona fasculata, zona reticularis, as well as directly under the adrenal capsule. Recently, the actions of autoantibodies to type 1 angiotensin II receptors have been described in patients with renal transplant rejection, with preeclampsia, and with primary hyperaldosteronism. The diagnostic role of antibodies in both forms of PHA (aldosterone-producing adenoma and bilateral hyperaldosteronism) requires clarification. Diagnosis and confirmation of the focus of aldosterone hypersecretion is a multi-stage procedure that requires a long time and economic costs. The relevance of timely diagnosis of primary hyperaldosteronism is to reduce medical and social losses. This work summarizes the knowledge about genetic mutations and presents all the original studies devoted to autoantibodies in PHA, as well as discusses the diagnostic capabilities and limitations of the available methods of primary and differential diagnosis of the disease and the prospects for therapy.
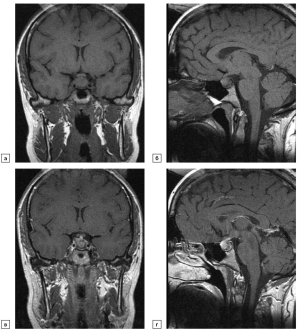
This article presents a literature review of the various forms of hypophysitis, its varieties, as well as the problem of radiation diagnosis and treatment of this pathology. Hypophysitis is a poorly understood and multifactorial disease which the difficulty of diagnosing is not only to a variety of nonspecific clinical manifestations and hormonal research data, but also the ambiguous results of MRI studies, the lack of clear MR patterns. The article reflects the main histological types of hypophysitis, the peculiarities of diagnosis in connection with general clinical symptoms, outlines the features of each type of hypophysitis with their own clinical observations. This review is devoted to modern ideas about the clinical course of hypophysitis, presented a set of characteristic diagnostic signs of the disease according to MRI and the treatment algorithms recommended today are also highlighted. The article summarizes data from foreign literature and our own clinical observations in order to develop an optimal protocol for MRI studies in patients with suspected hypophysitis, to develop recommendations for radiologists and endocrinologists for the correct results interpretation. The uniqueness of this review is the lack of data on the clinic, diagnosis and treatment of hypophysitis in the Russian literature today.
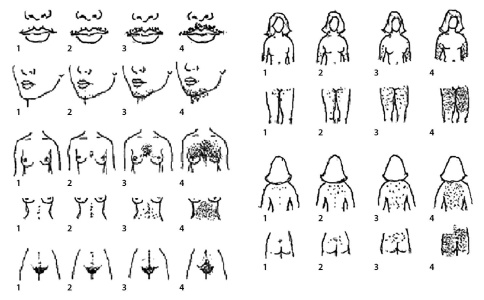
BACKGROUND: The basis for the management of transgender patients is the use of various hormonal correction schemes necessary for changing the hormonal sex and, possibly, further preparation for surgical correction. Currently, the choice of the starting dose and the scheme is carried out empirically, which lengthens the period of selection of therapy and increases the risk of its complications. Taking into account the individual characteristics of the patient can help in optimizing therapy.
AIM: Investigate Factors Affecting the Daily Demand for Testosterone Ester Blends in Transgender Men
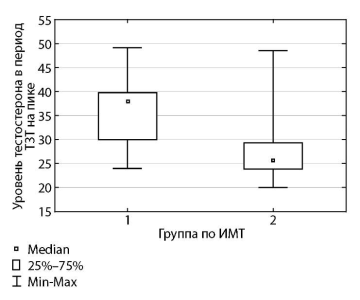
MATERIALS AND METHODS: This study is a case-control observational study. Patients included prior to initiation of testosterone replacement therapy. The analysis of factors interrelated with the daily requirement of testosterone preparations was carried out. Among the factors of interest, the body mass index (BMI), the results of blood tests for total testosterone and the functional state of the liver and kidneys are considered. Testosterone replacement therapy (TRT) regimens were evaluated in transgender men. For the calculation, we used the formulas for BMI and the average daily dose of testosterone. Based on the data obtained, conclusions were drawn that allow determining the necessary TRT scheme in different trans-gender men at an early stage of hormonal correction.
RESULTS: Our study included 58 transgender FtM patients who were prescribed testosterone preparations with an identical composition. We found a positive correlation between BMI and testosterone dose in patients of group II (p = 0.04).
CONCLUSION: In the conclusion, the obtained schemes of hormonal sex reassignment with a minimum risk of possible complications are presented. Our results demonstrated a relationship between BMI in overweight and obese patients and the need for TRT. For patients with a BMI of 25 to 29 kg / m2, the interval between injections of a mixture of testosterone esters does not differ significantly from that in the group with a BMI below 25 kg / m2 and averages once every 18 days, and in the group with a BMI ≥ 30 kg / m2 tested testosterone ester preparations should be prescribed once every 2 weeks (14 days).
BACKGROUND: In recent years, the demand for feminizing and masculinizing hormone therapy has increased significantly among transgender people around the world. There are no such studies in Russia and the amount of medical information on the transgender population is limited.
AIM: to assess the number of transgender patients who take hormone therapy without a doctor’s prescription and to characterize the medicines they use.
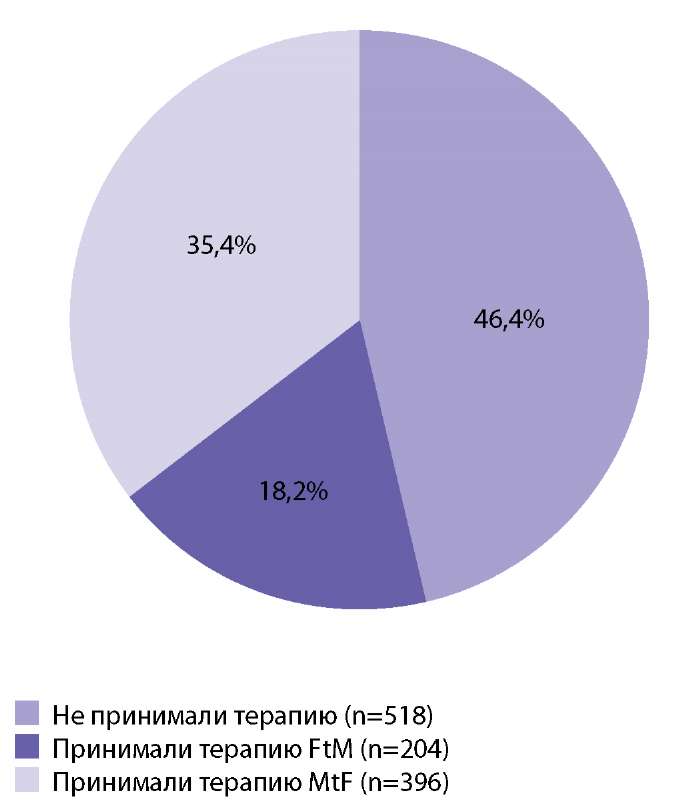
MATERIALS AND METHODS: data from 1117 transgender patients were included in to analysis: 44.01% (n=515) of them were trans women, 55.99% (n=630) were trans men. Patients applied to the “Scientific Center for Personalized Medicine” in order to receive medical care.
RESULTS: Half of transgender people (53.6%) are already taking hormonal drugs. More often transgender women (76.7%), less often transgender men (32.3%). In this case, only 8.6% turned to endocrinologists for the therapy prescription. Many patients used unlicensed drugs, use irrational schemes and combinations, often overdose.
CONCLUSION: A significant number of transgender people start using hormone replacement therapy on their own initiative, without the doctor’s supervision. The solution to this problem could be incensement of knowledge level in doctors and patients to create a friendly environment and productive interaction between therapists, endocrinologists and transgender people, as well as the organization of consulting centers within public medical institutions.
Dysphonia is a symptom of many endocrine pathologies. Hoarseness, voice fatigue, decrease of the voice pitch, reduce of the range are typical complaints for hypothyroidism, caused by an increased amount of polysaccharides and accumulation of fluid in the lamina propria of the vocal folds. An excess of growth hormone causes an overproduction of insulin-like growth factor-1, which leads to abnormalities in the craniofacial region and proliferation of the upper respiratory tract tissues, including thickening of the laryngeal cartilages, vocal folds and decreasing of the voice pitch. Hyperglycemia, changes in the balance of fluid and electrolytes in diabetes mellitus can indirectly affect the voice: xerostomia complicates phonation due to impaired hydration of the laryngeal mucosa, diabetic neuropathy often disrupts the work of the laryngeal muscles involved in voice formation. Voice changes are observed not only in endocrine disorders, but also during puberty, the phases of the menstrual cycle and during menopause. Laryngeal structures are modified under the influence of hormones and external factors, which generally changes pitch and intensity of the voice, timbre and resonance, articulation and prosodic characteristics. The purpose of this review is to summarize and systematize data on physiological and pathological voice changes in patients of different age groups and sex. The possibilities of a multidisciplinary approach to rational voice correction are demonstrated.
Carbohidrates metabolism disturbancies
BACKGROUND: There is a lack of data on the features of dysglycemia in hospitalized patients with COVID-19 and concomitant diabetes mellitus (DM) confirmed by continuous glucose monitoring (CGM).
AIM: to study the glycemic profile in hospitalized patients with COVID-19 and type 2 diabetes mellitus by continuous glucose monitoring and the role of steroid therapy in dysglycemiadevelopment.
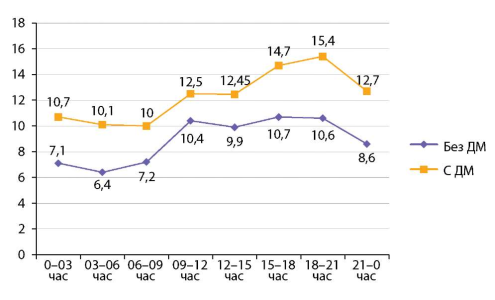
MATERIALS AND METHODS: We examined 21 patients with COVID-19 and DM 2 and 21 patients with DM 2 without COVID-19 (control group) using a professional 4–7-day CGM. We also compared two subgroups of patients with COVID-19 and DM 2: 1) patients received systemic glucocorticosteroids (GCS) during CGM and 2) patients in whomCGMwas performed after discontinuation of GCS.
RESULTS: Compared with controls, patients with COVID-19 and DM2 had lesser values of glycemic «time in range» (32.7 ± 20.40 vs 48.0 ± 15.60%, p = 0.026) andhigher parameters of mean glycemia (p <0.05) but similar proportion of patients with episodes of hypoglycemia (33.3% vs 38.1%, p = 0.75). Patients who received dexamethasone during CGM were characterized by higher hyperglycemia and the absence of episodes of hypoglycemia. In patients who hadCGM after dexamethasone discontinuation, hyperglycemia was less pronounced, but 60% of them had episodes of hypoglycemia, often nocturnal, clinically significant and not detected by routine methods.
CONCLUSION: Patients with COVID-19 and DM 2had severe and persistent hyperglycemia but a third of them hadalso episodes of hypoglycemia. During therapy with dexamethasone, they had the most pronounced hyperglycemia without episodes of hypoglycemia. In patients who underwent CGM after discontinuation of dexamethasone, hyperglycemia was less pronounced but 60% of them have episodes of hypoglycemia, often nocturnal, clinically significant and not diagnosed by routine methods. It would be advisable to recommend at least a 5–6-fold study of the blood glucose level (with its obligatory assessment at night) even for stable patients with COVID-19 and DM 2after the end of GCS treatment.
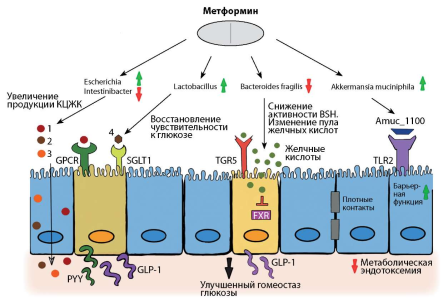
The gut microbiome is the largest microbial habitat in the human body. The main functions include obtaining energy from complex food fibers, maturation and formation of the immune system, intestinal angiogenesis, restoration of epithelial damage to the intestine, development of the nervous system, protection against pathogens, etc. It is also known that a number of drugs can cause changes in the composition of the intestinal microflora, and intestinal bacteria, in turn, produce a number of enzymes and metabolites that can chemically change the structure of drugs, leading to more side effects, and in some cases to positive changes. In this review we present current evidence supporting the effects of microbiota in host-drug interactions, in particular, the reciprocal effects of gut microbiota and oral hypoglycemic drugs on each other. Gaining and evaluating knowledge in this area will help pave the way for the development of new microbiota-based strategies that can be used in the future to improve treatment outcomes for type 2 diabetes mellitus (T2D).
Pediatric Endocrinology
McCune–Albright–Braitsev Syndrome (MAB syndrome) is a very rare multisystem disease manifested by fibrous bone dysplasia, coffee-and-milk colored spots, hyperfunction of various endocrine glands and a number of pathologies of other body systems. We present a description of a clinical case of a severe progressive course of MAB Syndrome in a nine-year-old girl. With this diagnosis, the girl is observation of the girl began when she was 2.5 years old, when spots of coffee-and-milk, polyosseous fibrous dysplasia, peripheral premature sexual development against a backdrop of estrogen-secreting ovarian cysts, multinodular goiter were detected. In the process of dynamic observation, it was noted that the child’s active growth stopped against a backdrop of deformities of the skeletal system with multiple repeated fractures of the extremities; progression of skull deformity with stenosis of the optic nerve canals and deterioration of visual acuity; development of STH hypersecretion, hypophosphatemic rickets, tachycardia. Appropriate suppressive / replacement therapy was prescribed for each of the endocrine dysfunctions. The article presents algorithms for examining a girl in dynamics, criteria for choosing a component-wise management tactics and a discussion of the features of the course of all manifestations of the Syndrome.
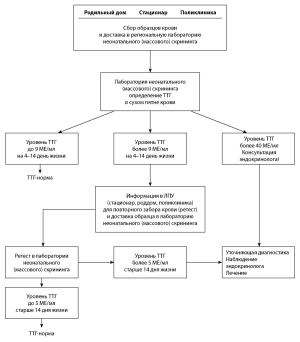
Congenital hypothyroidism is an important issue of pediatric endocrinology at which timely diagnosis and treatment can prevent the development of severe cases of the disease. The developed clinical guidelines are a working tool for a practicing physician. The target audience is pediatric endocrinologists and pediatricians. They briefly and logically set out the main definition of the disease, epidemiology, classification, methods of diagnosis and treatment, based on the principles of evidence-based medicine.
BACKGROUND: Hyperthyreoidism due to Graves’ disease is a rare disorder in pediatric practice. There is 2 treatment options in Graves’ disease: medical treatment and definitive treatment, including surgery and radioactive iodine. Each method has its advantages and disadvantages. If medical therapy is ineffective the choice between radical treatment method is raised: radioactive iodine or total thyroidectomy. In this research we analyze treatment outcomes in pediatric Graves’ disease patients after different radical treatment methods.
AIM: Comparative analysis of radical treatment outcomes in pediatric patients with Graves’ disease.
MATERIALS AND METHODS: Retrospective and prospective one-center research of 122 patients with Graves’ disease after radical treatment (between 2016 and 2021)
RESULTS: The mean age was 13.5±3,5 year at the moment of examination. Patients were divided into 2 groups due to the radical treatments method: 1 group (n=60) were children after surgical treatment, 2 group (n=62) — after radioactive iodine. The mean dose of medical treatment in these groups did not reliably differ (p=0,06), duration of the medical treatment was reliably longer in patients after radioactive iodine (p=0,024). Graves’ orbitopathy was diagnosed in 58 patients (47,5%) and met equally often in both groups, but active stage of Graves’ orbitopathy was diagnosed only in patients from the 1st group. Thyroid size was reliable bigger in patients from the 1st group (p=0,004), and thyroid gland nodes were diagnosed only in patients from 1st group (p=0,0007).
CONCLUSION: RI can be considered an effective and safe treatment for GD. The effectiveness of RI depends on the volume of the thyroid gland; according to the results of the constructed ROC curve, the risk of repeated RI is higher with a volume of more than 55 cm3. Also radioactive iodine is undesirable if there is signs of ophatalmopathy due to its possible deterioration. According to the results of the study hypoparathyroidism after surgical treatment was diagnosed in 20%, recurrent laryngeal nerve injury was diagnosed after surgical treatment in 5% of patients. In patients with identified nodular goiter according to the results of ultrasound, surgical treatment is preferable due to the impossibility of excluding thyroid cancer.
Reproductive Endocrinology
Polycystic ovary syndrome (PCOS) is a polygenic endocrine disorder caused by both genetic and epigenetic factors. Depending on the period of a woman’s life, the clinical picture, diagnosis, and treatment tactics of the disease are different. PCOS has a complex of reproductive, metabolic and psychological characteristics. The target audience of these clinical recommendations are obstetrician-gynecologists, endocrinologists, general practitioners, general practitioners. In these clinical guidelines, all information is ranked according to the level of persuasiveness of recommendations and the reliability of evidence, depending on the number and quality of studies on this issue.
According to present medical databases there many trials to provide in vivo researches in vivo to confirm/refute shortening process of telomeres among patients with Turner syndrome. Despite the successful clinical experience of providing such patients with Turner syndrome, a lot of omics (proteomic and metabolomic) aspects still stay unclear. Main disadvantages of most researches are small volume and minimized mathematical correlation with chronic disease (coronary heart disease, essential hypertension, cardiovascular malformations). Finally, organization of international prospective multi-centered researches in vivo including patients with mosaic cariotype and co-operation between physicians and biologists are optimal solutions for this present problem.
Obituary
On April 18, 2022, Professor Elvira Petrovna Kasatkina, Honored Doctor of the Russian Federation, Honorary Head of the Department of Pediatric Endocrinology of the RMANPO, Doctor of Medical Sciences, died at the age of 93.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2308-1430 (Online)










































.jpg)


