Clinical endocrinology
BACKGROUND: Timely referral of patients for genetic testing to rule out MEN1-associated primary PHPT is important factor in determining treatment strategy and prognosis. In the context of the limited availability of genetic testing, the search for clinical markers indicative of MEN1 gene mutations remains an extremely relevant task.
AIM: To determine the diagnostic value of clinical features of primary PHPT in young patients for predicting the presence of MEN1 gene mutations.
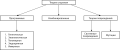
MATERIALS AND METHODS: A single-center, prospective study was conducted at the Endocrinology Research Centre, involving 273 patients with PHPT in the period 2015–2022. Based on the results of genetic and laboratory tests, patients were divided into three groups: those with MEN1 gene mutations (MEN+ group, n=71), those without MEN1 gene mutations — isolated sporadic PHPT (MEN- group, n=158), and patients with PHPT and associated endocrine gland disorders — MEN-1 syndrome phenocopies (PHEN group, n=32). Subgroups of patients younger than 40 years of age were also identified. Comparative analysis was performed among the independent groups and subgroups, and logistic regression analysis was used to develop a mathematical model for predicting the probability of the presence of MEN1 gene mutation.
RESULTS: Patients in the MEN+ and MEN- groups were comparable by gender and age at manifestation, as well as calcium-phosphorus metabolism parameters and PHPT complications. In the PHEN group, PHPT manifested at older age compared to the other groups (p<0.001 for all), with lower total calcium levels and a trend toward lower iPTH concentrations. The MEN+ group had a significantly higher frequency of multiglandular parathyroid (PG) involvement, PHPT recurrence, and positive family history compared to the MEN- and PHEN groups. Histologically, adenomas predominated in the PHEN and MEN- groups (92% and 94%, respectively), whereas hyperplasia of PGs were more common in the MEN+ group (49%). None of the PHEN patients had all three «classic» components of the MEN-1 syndrome, and the clinical course of PHPT was similar to that of the MEN- group. These differences were also observed in the subgroups of patients younger than 40 years, which formed the basis for the development of a mathematical model. The logistic regression equation for predicting the probability of the presence of the MEN1 gene mutation included eight predictors, with a diagnostic sensitivity of 96% and specificity of 98%.
CONCLUSION: Based on the analysis performed, eight hereditary predictors of PHPT within the MEN-1 syndrome were identified. A mathematical model was developed to predict the presence of the MEN1 gene mutation in patients, which demonstrated high classification performance on the training dataset. Further refinement of the model will help improve the quality of medical care for patients with PHPT.
BACKGROUND: Data on the effect of 131I on the course of Graves’ orbitopathy (GO) are contradictory. A number of studies indicate a deterioration in the course of GO against the background of RAIT, in other studies such a connection has not been established. Cytokines that regulate inflammation could potentially be biomarkers for assessing GO activity and predicting the course of GO after RAIT.
AIM: The purpose of this study was to evaluate the dynamics of eye symptoms and analyze immunological parameters: cytokine TGF-β1 and cytokine receptors: sTNFα-R1, sTNFα-R2, sIL-2R, sIL-6R over time after RAIT, as possible predictors of GO activation.
MATERIALS AND METHODS: The study included 59 patients (118 orbits) with GD in the state of euthyroidism and subclinical hyperthyroidism and low active and inactive GO, aimed at conducting RAIT. Concentrations of cytokine TGF-β1, sTNFα-RI and sTNFα-R2, sIL-2R, sIL-6R, TSH receptor antibodies (rTSH-Ab), free thyroxine (FT4) and free triiodothyronine (FT3), thyroid-stimulating hormone (TSH) in the blood serum were determined. Ultrasound examination of the thyroid gland, multispiral computed tomography (MSCT)/magnetic resonance imaging (MRI) of the orbits was performed. The examination was carried out 3, 6, 12 months after the RAIT.
RESULTS: The deterioration of the course of the GO (1–2 points according to CAS) was noted after 3 months. (32.5%) and to a lesser degree after 6 and 12 months (13.2% and 8.45%, respectively). Dynamics were not noted, approximately, in the same number of patients (40.5%, 41.5%, 45.8%, respectively). An improvement in the course of the GO was noted after 6 and 12 months (45.3, 45.8, respectively). After 3 and 6 months, the achievement of hypothyroidism and a significant increase in the level of rTSH-Ab were noted. In the analysis of cytokines and their receptors a significant decrease in the level of TGF-β1 was noted after 3, 6 and 12 months. There was also a significant decrease in sTNF-R1 and sIL-2R at 3 and 6 months. The level of sTNFα-R2 significantly decreased 3 months after RAIT. The level of sIL-6R has not changed significantly. After 3 months in patients with positive dynamics of image intensification, the level of TGF-β1 did not significantly change compared with the level before RAIT, in patients with worsening of the course of GO or without dynamics, the level of TGF-β1 significantly decreased. After 6 months, there was the same trend, not reaching statistical significance. The IgG4 level and the IgG4/IgG ratio increased to 6 and 12 months, which corresponded to an increase in diplopia index.
CONCLUSION: The main limiting factor in the conduct of RAIT is the activity of the autoimmune process in the orbits. Since patients with inactive (CAS 0–2) or low activity (CAS 3–4) GO were referred for RAIT, there was no pronounced activation of GO after RAIT. There was a slight deterioration in the course of GO by only 1–2 points according to CAS after 3 months. (32.5%) and to a lesser degree after 6 months (13.2%). In the study, it was found that the main predictors of the deterioration of the course of GO after RAIT are uncompensated hypothyroidism, a high level of rTSH-Ab and a decrease in the level of cytokine TGF-β1.
Introduction: Tumor-induced osteomalacia is an acquired rare disease manifested by hypophosphatemic osteomalacia due to excessive secretion of fibroblast growth factor 23 (FGF23). FGF 23 is a non-classical hormone secreted by bone tissue (osteocytes) and regulates phosphorus metabolism.
The aim of this work is to present clinical experience in the diagnosis, treatment and rehabilitation of patients with tumor-induced osteomalacia.
Materials and methods: 40 patients with clinically-confirmed tumor-induced osteomalacia were included in the study, 34 of whom had the tumor localized, 27 underwent surgical treatment and 21 achieved stable remission.
Results: The median age was 48 [41; 63] years, 43% were men, the time left from the the onset of the disease was 8 [4; 10] years. Biochemical findings were hypophosphatemia 0.47 [0.4; 0.53] mmol/l, a decrease in the tubular reabsorption phosphate 62 [52; 67]%, and an increase in alkaline phosphatase of 183 [112; 294] units/l. At the time of diagnosis, 100% had multiple pathological fractures, only 10% could move independently, and 77.5% classified the pain as unbearable (8–10 points according to the 10-point pain syndrome scale ). Among the methods used to detect tumors, the most sensitive were scintigraphy with tectrotide with SPECT/CT 71.4% (20/28) and MRI 90% (18/20). In 35% of cases, the tumor was localized in soft tissues and in 65% in bone tissue; The tumor was most often detected in the lower extremities, followed by the head in frequency of localization. 18 patients currently have no remission and they receive conservative treatment (phosphorus and alfacalcidol n=15 and burosumab n=3). In case of achieving remission (n=21), regression of clinical symptoms and restoration of bone and muscle mass was observed. Extensive excision of the tumor without prior biopsy resulted in the best percentage of remission — 87%.
Conclusion: Tumor-induced osteomalacia is characterized by severe damage to bone and muscle tissue with the development of multiple fractures, muscle weakness and severe pain syndrome. In laboratory diagnostics, attention should be paid to hypophosphatemia, a decrease in the tubular reabsorption phosphate index and increased alkaline phosphatase. The use of functional diagnostic methods with a labeled somatostatin analogue to the subtype 2 receptor and MRI with contrast enhancement are the most accurate methods of topical diagnostics. In case of localization of the tumor, a wide excision without a preliminary biopsy is recommended.
This review article contains a summary of modern aspects of preoperative preparation, surgical treatment, and follow-up of patients with adrenal pheochromocytomas. The main component of preoperative preparation is the use of alpha-blockers. The need to prescribe them to all patients is increasingly disputed, especially for patients without severe hypertension. An increasing number of publications demonstrate positive results of treatment without the use of alpha-blockers, advocating an individual approach and the use of the drug according to certain indications. Minimally invasive endoscopic techniques of adrenalectomy have become widespread in surgical treatment. They are represented by laparoscopic and retroperitonescopic technic, including using their single-port modifications. The earliest possible intersection of the central vein in the past was considered the most important aspect of adrenalectomy for pheochromocytoma, currently, due to the development of surgical techniques and anesthesiological manuals, this has ceased to be a mandatory rule of successful surgery. Despite the significant influence of the intersection of this vessel on intraoperative hemodynamics, surgical tactics with its later intersection have their own justifications and do not lead to a deterioration in treatment results. The standard volume of surgical intervention for pheochromocytomas is total adrenalectomy, however, in the presence of hereditary syndromes, such as multiple endocrine neoplasia type 2 syndrome, neurofibomatosis type 1, von Hippel-Lindau syndrome, it is possible to perform cortical-sparing adrenalectomy.
Ageing (as known as eldering, senescence) is a genetically and epigenetically programmed pathophysiological process. Velocity of biological ageing is defined as balance between alteration and reparation of body structures. According to last World Health Organization (WHO) highlights ageing still stays an extremely actual scientific, social and demographic problem: in 2020 total number of people older than 60 years and older was 1 billion people; in 2030 future number may be 1,4 billion people, in 2050 — 2,1 billion people. Absence of single universal theory of aging nowadays is reason for scientifical and clinical collaboration between biologists and doctors, including endocrinologists. Designing of potentially effective newest anti-ageing strategies (such as natural/synthetic telomerase regulators, mesenchymal stem cells etc.) is of interest to scientific community. The aim of present article is a review of modern omics (genomic, proteomic, metabolomic) ageing mechanisms, potential ways of targeted prevention and treatment of age-related disease according to conception of personalized medicine. Present review is narrative, it does not lead to systematic review, meta-analysis and does not aim to commercial advertisement. Review has been provided via PubMed article that have been published since 1979 until 2022.
A clinical case of a man 66 y.o. who was diagnosed with hormone-inactive pituitary macroadenoma complicated by corneal erosion and partial atrophy of the optic nerve of the left eye due to exophthalmos. The increase in prolactin level was regarded due to a «stalk-effect». The patient underwent a transnasal pituitary adenomectomy with subsequent regression of symptoms. After 4 years, against the background of a new coronavirus infection, increasing general weakness, headaches, a crisis increase in blood pressure and tachycardia attacks appeared. Computed tomography (CT) accidentally revealed an adrenal incidentaloma, in laboratory tests — hypercortisolism, elevated ACTH levels, hypokalemia, hyperglycemia, increased levels of metanephrine and normetanephrine. The patient developed acute steroid psychosis, after which an adrenalectomy with a tumor was performed, a pheochromocytoma was histologically confirmed. After surgery, there was a regression of symptoms, the development of adrenal insufficiency with reduced levels of ACTH and cortisol. Upon further examination, a polynodose euthyroid goiter was established, the biopsy of the nodes — Hashimoto’s thyroiditis (Bethesda II). Meanwhile, primary hyperparathyroidism was detected. According to ultrasound, scintigraphy with Ts99m-Technetril and CT revealed an increase of left parathyroid gland. A bilateral revision of the neck, removal of the right upper and left upper parathyroid adenomas were performed. In the postoperative period, the levels of calcium and parathyroid hormone were normalized. Given the presence of a combination of multiple tumors of the endocrine system (primary hyperparathyroidism, corticotropin-producing pheochromocytoma, hormone-inactive pituitary macroadenoma, polynodose euthyroid goiter), the MEN1 syndrome was clinically established. The study of 2 and 10 exons of the MEN1 gene revealed no mutations, which does not exclude the presence of a hereditary syndrome. The patient continues observation. In the available literature in Russian and English languages the case of ACTH pheochromocytoma as part of the MEN type 1 syndrome have not been found. Therefore, we consider the presented case to be the first one.
Reset osmostat syndrome (ROS) is characterized by a change of normal plasma osmolality threshold (decrease or increase), which leads to chronic dysnatremia (hypo- or hypernatremia). We have described a clinical case of ROS and chronic hyponatremia in a patient with chordoid glioma of the III ventricle. It is known that the patient had previously been diagnosed with hyponatremia (131–134 mmol/l). She has not hypothyroidism and hypocorticism. There is normal filtration function of the kidneys was (CKD-EPI 91.7 ml/mi/1,73m2). Urine osmolality and sodium level were studied to exclude of concentration kidney function disorder. During first three days after removal of the tumor of the third ventricle (chordoid glioma, WHO Grade II), the sodium level decreased to 119 mmol/l. Repeated infusions of 200–300 ml hypertonic 3% sodium chloride solution, gluco- and mineralocorticoid therapy was ineffective, increasing plasma sodium levels by 2–3 mmol/l with the return to the initial level during 6–8 hours. Hypopituitary disorders did not develop after surgery. With further observation, the sodium level remained within 126–129 mmol/l for 6 months after surgery. The water load test make exclude the classic syndrome of inappropriate secretion of antidiuretic hormone, and confirmed the diagnosis of RSO. Because of absence of clinical symptoms associated with hyponatremia, no medical correction was required, patient was recommended to clinical follow-up.
Carbohidrates metabolism disturbancies
Recent studies show that Alzheimer’s disease (AD) has many common links with conditions associated with insulin resistance, including neuroinflammation, impaired insulin signaling, oxidative stress, mitochondrial dysfunction and metabolic syndrome. The authors conducted an electronic search for publications in the PubMed/MEDLINE and Google Scholar databases using the keywords “amyloid beta”, “Alzheimer type-3-diabetes”, “intranasal insulin”, “metformin”, “type 2 diabetes mellitus”, “incretins” and “PPARy agonists». A systematic literature search was conducted among studies published between 2005 and 2022. The authors used the following inclusion criteria: 1) Subjects who received therapy for AD and/or DM2, if the expected result concerned the risk of cognitive decline or the development of dementia; 2) The age of the study participants is > 50 years; 3) The type of studies included in this review were randomized clinical trials, population-based observational studies or case-control studies, prospective cohort studies, as well as reviews and meta-analyses; 4) The included articles were written in English. In recent years, there has been considerable interest in identifying the mechanisms of action of antidiabetic drugs and their potential use in AD. Human studies involving patients with mild cognitive impairment and Alzheimer’s disease have shown that the administration of certain antidiabetic drugs, such as intranasal insulin, metformin, incretins and thiazolidinediones, can improve cognitive function and memory. The purpose of this study is to evaluate the effectiveness of antidiabetic drugs in the treatment of AD. According to the results of the study, metformin, intranasal insulin, thiazolidinediones and incretins showed a positive effect both in humans and in animal models. Recent studies show that thiazolidinediones can activate pathways in the brain that are regulated by IGF-1; however, rosiglitazone may pose a significant risk of side effects. The results of clinical studies on the use of metformin in AD are limited and contradictory.
BACKGROUND: Diabetes mellitus (T2DM) is a serious medical and social problem. Now they are studying the possibility of a new stratification of diabetes. The possibility of cluster analysis for different durations of diabetes, in different cohorts to identify phenotypic clusters of T2DM and validation by reproducing clusters is relevant.
AIM: Identify clusters of type 2 diabetes mellitus in patients with different disease duration based on five variables: HbA1c, age at diagnosis, BMI, HOMA-IR, HOMA-B and study the clinical features and complication rates in each cluster in the Novosibirsk region.
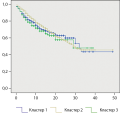
MATERIALS AND METHODS: Cluster analysis of K-means was performed in 2131 patients with T2DM, aged 44 to 70 years, with a duration of diabetes of 6.42±5.66 years, living in the Novosibirsk region based on 5 variables — HbA1c, age at diagnosis, BMI, HOMA-IR, HOMA-B. All patients a complete clinical and laboratory examination. The insulin resistance index in the HOMA (HOMA-IR, u) and the β-cell function assessment index (HOMA-B) were calculated using the calculator version 2.2.3 at www.dtu.ox.ac.uk.
RESULTS: Cluster analysis revealed: Cluster 1 included 455 patients with preserved β-cell function (HOMA-B 82.97±23.28%), moderate insulin resistance (HOMA-IR 5.57±4.72) and higher diastolic BP; Cluster 2 in 1658 patients with reduced function of β-cells (HOMA-B 21.71±12.51%), the lowest indices of insulin resistance (HOMA-IR 3.50±2.48) and was characterized by a longer duration of diabetes, high fasting glycemia , HbA1c, higher eGFR and MAU, men compared with women had a 31% higher risk of developing diabetic neuropathy and 28% more diabetic nephropathy; Cluster 3 in 18 patients with high function of β-cells (HOMA-B 228.53±63.32%), severe insulin resistance (HOMA-IR 6.92±4.77), features were high incidence of men, shorter duration of diabetes, lower fasting glycemia and HbA1c, lower diastolic BP and eGFR, high incidence of early development of diabetic retinopathy after 4.00±3.6 years.
CONCLUSION: Cluster analysis in patients with different durations of diabetes mellitus confirmed the possibility of using cluster analysis to identify T2DM phenotypes in the Russian population. The clusters differed in the clinical characteristics of patients, the frequency and risk of diabetic complications. These results have potential value for early stratification of therapy.
Background. The undoubted importance of this work lies in the fact that for the first time in the Republic of Kazakhstan, an analysis is being made of the relationship between age and treatment outcome in patients with a comorbid diagnosis of tuberculosis and diabetes mellitus.
Purpose of the study. Identification of the correlation between the age of patients with tuberculosis with diabetes mellitus and the outcome of treatment.
Materials and methods. Cross-sectional retrospective study of 2,125 patients with TB and diabetes mellitus out of a total of 43,807 of all patients diagnosed with TB (2017-2019). The study analyzed the data of patients with comorbidity from all regions of Kazakhstan (data from 14 regions and 3 cities of republican significance) (2017-2019).
Results. A high prevalence of tuberculosis morbidity with a concomitant diagnosis of diabetes mellitus in the age group from 45 to 64 years was revealed. This group consisted of 1193 patients out of 2115 (56.4% of the total number of patients with tuberculosis and diabetes mellitus). The average age of all studied patients with DM was 54.7±13.4 years. There is a positive correlation between age and treatment outcome in TB patients. Mortality was higher in the age group over 45 years old – OR95%CI = 0.213 [0.019–2.362], p – 0.0000015 (p < 0.05).
Pediatric Endocrinology
Cryptorchidism is the most frequent congenital disorders of the reproductive system, is present in 2–3% of term newborn boys. Genes involved in embryonic testicular migration are known but their role in cryptorchidism development are not investigated enough. Genetical causes of cryptorchidism are identified in 5–7% of patients. The article contains data on the role of insulin-like peptide 3 and its receptor, anti-Müllerian hormone, gonadotropins, androgens in embryonic testicular migration. INSL3 and AMH are presented as markers of testicular dysfunction associated with cryptorchidism. Hypogonadotropic hypogonadism is also associated with cryptorchidism and can be diagnosed based on it. Results of modern investigations determine the necessary of hormonal and genetical examination of patients with isolated cryptorchidism to detect causes of cryptorchidism and manage of patients.
Reproductive Endocrinology
Polycystic ovary syndrome (PCOS) is one of the most pressing problems in endocrine gynecology. The main signs of the disease are hyperandrogenism, menstrual and/or ovulatory dysfunction, and polycystic ovarian structure according to ultrasound. Women with PCOS are at risk for developing metabolic syndrome, type 2 diabetes, cardiovascular disease, and endometrial cancer. In this connection, the pathogenetic mechanisms of the occurrence of this syndrome are continuously studied and new methods of treatment are being sought. PCOS is characterized by a wide range of various disorders of the neuroendocrine regulation of the reproductive system. The main focus of the review is aimed at summarizing information about the etiological role of neuropeptides and neurotransmitters, such as phoenixin, galanins, orexins, GABA, in the pathophysiology of PCOS and about the possibility of their use for diagnostic and therapeutic purposes. In recent decades, the interest of scientists has been focused on the study of KNDy neurons, because it is the kisspeptin synthesized by them that is one of the main regulators of the hypothalamic-pituitary-ovarian axis. This article discusses data on the significance of KNDy neurons in the pathogenesis of the syndrome. Information is provided on the effect of elevated levels of androgens and anti-Müllerian hormone on GnRH neurons. Also analyzed are studies on functional and structural disorders in the hypothalamus in PCOS. Literature search was carried out in national (eLibrary, CyberLeninka.ru) and international (PubMed, Cochrane Library) databases in Russian and English. The priority was free access to the full text of articles. The choice of sources was prioritized for the period from 2018 to 2023.However, taking into account the insufficient knowledge of the chosen topic, the choice of sources dates back to 1998.
Clinical guidelines
Menopausal symptoms can disrupt the life course of women at the peak of their career and family life. Currently, the most effective treatment for these manifestations is menopausal hormone therapy (MHT). The presence of cardiovascular and metabolic diseases in itself does not exclude the possibility of prescribing MHT to relieve menopausal symptoms and improve quality of life. However, often an obstacle to the use of this type of hormonal therapy is the fear of doctors who are afraid of doing more harm to patients than good. Caution is especially important when it comes to women with underlying health conditions. Moreover, it should be recognized that there is a lack of high-quality research regarding the safety of MHT for major chronic non-infectious diseases and common comorbid conditions. The presented consensus document analyzed all currently available data obtained from clinical trials of various designs and created a set of criteria for the acceptability of prescribing MHT to women with concomitant cardiovascular and metabolic diseases. Based on the presented document, doctors of various specialties who advise women in menopause will receive an accessible algorithm that will allow them to avoid potentially dangerous situations and reasonably prescribe MHT in real practice.

This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License (CC BY-NC-ND 4.0).
ISSN 2308-1430 (Online)















































.jpg)


